
Liver gates to access everywhere in the liver: how can we learn?
Introduction
Minimally invasive liver surgery (MILS) has exponentially increased in the last few years. Both in its laparoscopic and robotic variations, the number and the complexity of the procedures are rising up. Since the first laparoscopic left lateral sectionectomy, published in 1996 (1,2), a wide number of techniques have been published. The First Consensus Meeting held in Louisville in 2009 settled the basis of the incoming future of MILS (3). In 2014, the Consensus Meeting held in Morioka raised new incoming concepts such as caudal approach, vein-guided dissections and a renewed interest in the extraglissonean approach (4).
In 1986, Takasaki reported the whole control of the Glissonean pedicle without dissecting the portal vein, hepatic artery, and bile duct. In this approach, the hilar fascia is kept intact and liver pedicles are clamped and sectioned from the liver hilum (5). Certainly, one of the main advantages of this technique is that potential damage to hilar structures is avoided. By accessing the hilum, pedicles to hemilivers, sectors and individual segments can be dissected and encircled. In the last decades, many studies and randomized trials have been published highlighting the feasibility and reproducibility of the Glissonean pedicle approach (6,7). Both approaches have been routinely performed in traditional open major hepatectomy. In the last decade, these techniques have been widely refined for minimally invasive procedures (8,9). We will explain how Glissonean approach may be performed during laparoscopic liver surgery and how to achieve precise control of pedicles for adequate anatomical resections.
The modern conception of Glissonean approach
Very recently, the Tokyo Guidelines on Minimally Invasive Liver Surgery have updated the anatomical concepts of the 2000 Brisbane Terminology and have given clear instructions about what is considered anatomical resection and Glissonean approaches (10). The most important definitions and recommendations are as follows:
- The Glissonean approach is a reasonable technique during minimally invasive anatomic liver resection (MIALR).
- During formal left and right hepatectomies using the Glissonean approach, it is safe to isolate and divide the 2nd order portal pedicles for inflow control. For the isolation of the 2nd and 3rd order portal pedicles during MIALR, the Glissonean approach appears to be more feasible than individual vessels and biliary ducts isolation.
There is a concept called “Gate Theory” in performing Glissonean pedicle isolation. According to this theory, Glissonean pedicle isolation is possible by maximizing the benefits of laparoscopic surgery (11).
Recognizing the following structures (Rouviere’s sulcus, cystic plate, umbilical plate, Arantius plate, and the Glissonean pedicle of the caudate process) as a landmark to isolate the Glissonean pedicle during MIALR is recommended.
Recognizing Laennec’s capsule as a landmark to isolate the extrahepatic Glissonean pedicles during MIALR is recommended.
Strategies to access the liver hilum by Glissonean approach
It should be kept in mind that the main aims when performing a hepatectomy (and mostly a minimally invasive hepatectomy) are:
- To keep patient’s safety independent of the approach.
- To minimize blood loss for postoperative recovery and for oncological reasons.
- To minimize the risk of bile leak to reduce the length of stay and postoperative infections.
To keep ischemic areas as small as possible as they may have an impact on postoperative recovery and oncological success (12).
To preserve as much parenchyma as possible in order to avoid postoperative liver insufficiency and to ensure enough volume for potential recurrence mostly in cases of metastases.
To keep oncological margins adequate and try to minimize the rate of R1 and R2 resections unless vascular R1 which is considered equal to R0 whenever vascular invasion is discarded.
There are two main strategies to access pedicles in order to perform anatomic hepatectomies (Figure 1):
- To open the fascia and approach portal, arterial and biliary structures individually (intrafascial or intraglissonean approach).
- To keep fascia intact and encircle portal pedicles without dissecting individual structures (extrafascial or Glissonean approach). This approach can be divided in further two approaches.
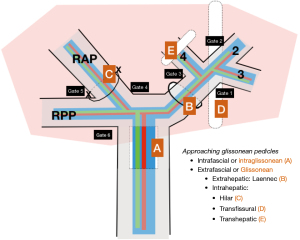
Both abovementioned approaches have advantages and disadvantages and should be kept in the armamentarium of the surgeon to improve the success rate for a proper and safe hepatectomy. During hilar approach, the individual dissection of structures of the first-order portal pedicles can be safely performed, even during minimally invasive access. However, 2nd order or more peripheral pedicles may be troublesome for this approach as hilar plate must be dissected really proximal and potential injury may be caused to other structures. On the contrary, it has been well-defined the safety of the Glissonean approach for 2nd and 3rd order divisions on both sides, minimizing the risks of anatomical variations at this level. We strongly advocate for a precise preoperative planification including 3D reconstructions to properly plan an adequate surgical strategy (13).
A progressive and carefully monitored learning curve is strongly recommended. The access to liver gates is different considering left or right sides. The left gates (1, 2 and 3) and access to them is probably the best starting point. In this area, left lateral segmentectomies or left hepatectomies are strongly encouraged to be practices before moving to the right side. In the right side, Rouviere’s sulcus is probably a next level area from which isolating right posterior pedicle by encircling from Gates 5 to 6. In our opinion, and considering current difficulty scoring scales, right anterior sectionectomy and accessing from Gates 4 to 5 is the most difficult one and should be considered only for expert laparoscopic liver surgeons (14).
Our main recommendations for performing a safe Glissonean approach are:
- For first order division:
- For left-sided bifurcation, it is recommended to dissect from Gate 3 to Gate 1. Gate 3 is easily found just to the right of the falciform ligament above the hilar plate (15). Gate 1 should be found above G1 and Arantius ligament. An oblique approach from Gate 3 to Gate 1 may be useful to avoid damage to the posterior part of the left pedicle (
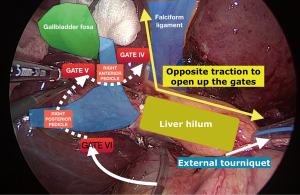
Video 1). - For primary bifurcation on the right side, a potential access is dissecting Gate 6 above G1R and moving upwards towards Gate 4. This approach has been widely used with good results. However, there is a potential risk in damaging bile duct as it usually divides further above the right portal vein bifurcation. To prevent this potentially harmful event, two maneuvers have been proposed: first, to pull firmly from the external tourniquet to stretch the hilar plate and be able to do the section of the right pedicle safely (16); and second, to make individual sections of right posterior and right anterior pedicles (Figure 2), moving from Gates 6 to 5 and from Gates 5 to 4, respectively (17,18).
- For left-sided bifurcation, it is recommended to dissect from Gate 3 to Gate 1. Gate 3 is easily found just to the right of the falciform ligament above the hilar plate (15). Gate 1 should be found above G1 and Arantius ligament. An oblique approach from Gate 3 to Gate 1 may be useful to avoid damage to the posterior part of the left pedicle (
- For second order division:
- When moving towards 2nd order division, accessing the Gates of Sugioka seems an even safer approach to avoid damage to other structures. In the left side, accessing the second order division is the most useful and safe technique for a left lateral sectionectomy. In this sense, transfissural approach using the falciform ligament landmark may clearly lead to the left lateral pedicle and ensure a safe section using a staple (
Video 2). However, this approach is also the easiest strategy to reach up to G3 and make an individual anatomical segmentectomy ( Video 3). - On the right-sided 2nd order division, it is mandatory to get excellent preoperative planification by angiographic computed tomography (angio-CT) scan, magnetic resonance imaging (MRI) and cholangio-MRI. Our protocol also includes preoperative 3D reconstruction to ensure perfect preoperative knowledge of all anatomic variations. For this area, we strongly advocate for Glissonean approach using Gates 4–6. From Gates 4 to 5 for a right anterior sectionectomy and from Gates 5 to 6 for a right posterior sectionectomy. Using the Laennec’ capsule or not will just depend on several factors, mainly personal experience, cirrhotic liver, steatosis, neoadjuvant chemotherapy and previous surgeries. Cirrhotic livers are very prone for a Glissonean approach using the Laennec’s capsule as this is usually thicker (
Video 4). On the contrary, steatotic grafts and postchemotherapy are more difficult and usually a hilar Glissonean transhepatic approach is usually preferred as Laennec’s capsule disrupts easily. - To approach Gates 4 and 5, “Cystic plate cholecystectomy” is often useful especially in performing a right anterior sectionectomy, S8 subsegmentectomy and S5 subsegmentectomy. The gallbladder including the cystic plate is pulled to develop a good view of hepatic hilum. It brings the good countertraction to the right anterior Glissonean pedicle (19).
- Central hepatectomy includes resection of medial and right anterior sectors. It is considered one of the most difficult laparoscopic liver resections. It has been clearly standardized by using hilar approach accessing Gate 3 and Gates 4 to 5. This approach may preclude iatrogenic damage to left and right posterior pedicles (20).
- When moving towards 2nd order division, accessing the Gates of Sugioka seems an even safer approach to avoid damage to other structures. In the left side, accessing the second order division is the most useful and safe technique for a left lateral sectionectomy. In this sense, transfissural approach using the falciform ligament landmark may clearly lead to the left lateral pedicle and ensure a safe section using a staple (
- For third order divisions and cone units dissection:
- Third order division needs Glissonean approach as dissection of individual structures seems too risky and unnecessary. Approaching third order pedicles by hilar approach is complex and needs advanced training and expertise. It is strongly advisable to approach second order branches, encircle and the move towards third order branches although this is variable and depends on personal experience and individual anatomy. All individual Glissonean pedicles can be accessed from the hilum using both Laennec’s capsule or intrahepatic. It is interesting to note that, if necessary, both approaches can be combined and start with a hilar approach for a main tertiary pedicle and then move transhepatic to find a closer pedicle from a cone unit that may complement a precise anatomical resection (Figure 1 and 9,21).
- It should also be considered that transhepatic approach may be highly useful for performing anatomical parenchymal sparing resections by performing precise clamping of specific anatomical areas. It is really convenient in segments 6–7, in which transhepatic approach following the root of right hepatic vein leads to G7 in a very easy-to-standardize way (22,23).
- Transhepatic approach is probably the best way to approach cone units in peripheral areas. Rather than performing a non-anatomical ultrasound-guided resection, it is a valid and elegant option to locate individual pedicles that may combine cone units which should be resected in order to fully include the tumor with negative margins (
Video 6). This approach is particularly useful and easy in the visceral surface of segments 6–7 and 2–3.
Conclusions
A very recent survey preparatory for the Tokyo 2020 Guidelines performed on more than 500 hepatobiliary surgeons showed that nearly half of them had never performed a Glissonean approach for a laparoscopic liver resection (24). The abovementioned maneuvers require experience and adequate training but are very much appropriate for achieving optimal results and precise anatomical resections. The gate-guided strategy is useful for both laparoscopic and open approaches and a perfect knowledge of the gates may be a useful tool to be kept in the mind of junior and experienced liver surgeons. It should, however, be noted that this strategy is just that. It should not replace proper intraglissonean dissection when needed, mostly in cases of tumours very close to the hilum, perihilar biliary tumors and in those cases in which lymphadenectomy should be done meticulously. However, we consider that this strategy is the most adequate for left-sided first order division, for secondary-order division and for third-order division (this last one only in very experienced hands).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Edoardo Rosso and Santiago Azagra) for the series “Focus on Technical Advancement in Mini-invasive HPB Surgery” published in Digestive Medicine Research. The article has undergone external peer review.
Peer Review File: Available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-66/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dmr.amegroups.com/article/view/10.21037/dmr-22-66/coif). The series “Focus on Technical Advancement in Mini-invasive HPB Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this article were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this article accompanying images and videos.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Azagra JS, Goergen M, Gilbart E, et al. Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc 1996;10:758-61. [Crossref] [PubMed]
- Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery 1996;120:468-75. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Takasaki K, Kobayashi S, Tanaka S, et al. Highly anatomically systematized hepatic resection with Glissonean sheath code transection at the hepatic hilus. Int Surg 1990;75:73-7. [PubMed]
- Takasaki K. Glissonean pedicle transection method for hepatic resection: a new concept of liver segmentation. J Hepatobiliary Pancreat Surg 1998;5:286-91. [Crossref] [PubMed]
- Figueras J, Lopez-Ben S, Lladó L, et al. Hilar dissection versus the "glissonean" approach and stapling of the pedicle for major hepatectomies: a prospective, randomized trial. Ann Surg 2003;238:111-9. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Berardi G, Igarashi K, Li CJ, et al. Parenchymal Sparing Anatomical Liver Resections With Full Laparoscopic Approach: Description of Technique and Short-term Results. Ann Surg 2021;273:785-91. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. The Tokyo 2020 terminology of liver anatomy and resections: Updates of the Brisbane 2000 system. J Hepatobiliary Pancreat Sci 2022;29:6-15. [Crossref] [PubMed]
- Sugioka A, Kato Y, Tanahashi Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec's capsule: proposal of a novel comprehensive surgical anatomy of the liver. J Hepatobiliary Pancreat Sci 2017;24:17-23. [Crossref] [PubMed]
- Yamashita S, Venkatesan AM, Mizuno T, et al. Remnant Liver Ischemia as a Prognostic Factor for Cancer-Specific Survival After Resection of Colorectal Liver Metastases. JAMA Surg 2017;152:e172986. [Crossref] [PubMed]
- Morimoto M, Tomassini F, Berardi G, et al. Glissonean approach for hepatic inflow control in minimally invasive anatomic liver resection: A systematic review. J Hepatobiliary Pancreat Sci 2022;29:51-65. [Crossref] [PubMed]
- Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 2016;5:281-9. [Crossref] [PubMed]
- Rotellar F, Pardo F, Benito A, et al. A novel extra-glissonian approach for totally laparoscopic left hepatectomy. Surg Endosc 2012;26:2617-22. [Crossref] [PubMed]
- Rotellar F, Pardo F, Benito A, et al. Totally laparoscopic right-lobe hepatectomy for adult living donor liver transplantation: useful strategies to enhance safety. Am J Transplant 2013;13:3269-73. [Crossref] [PubMed]
- Ciria R, Ayllón MD, Padial A, et al. Totally Laparoscopic Tourniquet ALPPS: Technical Standardization by Combining the Pure Hanging Maneuver and the Approach Through the Sugioka Gates. Ann Surg Oncol 2022;29:2410-1. [Crossref] [PubMed]
- Ciria R. ASO Author Reflections: Technical Steps for the Standardization of Laparoscopic Liver Tourniquet as a Modified ALPPS Procedure: A Feasible Option with Equivalent Results and Reduced Aggressiveness. Ann Surg Oncol 2022;29:2412-3. [Crossref] [PubMed]
- Tokumitsu Y, Tamesa T, Shindo Y, et al. Application and utility of surgical techniques for cystic plate isolation in liver surgery. Ann Gastroenterol Surg 2022;6:726-32. [Crossref] [PubMed]
- Rotellar F, Martí-Cruchaga P, Zozaya G, et al. Standardized laparoscopic central hepatectomy based on hilar caudal view and root approach of the right hepatic vein. J Hepatobiliary Pancreat Sci 2020;27:E7-8. [Crossref] [PubMed]
- Berardi G, Wakabayashi G, Igarashi K, et al. Full Laparoscopic Anatomical Segment 8 Resection for Hepatocellular Carcinoma Using the Glissonian Approach with Indocyanine Green Dye Fluorescence. Ann Surg Oncol 2019;26:2577-8. [Crossref] [PubMed]
- Honda G, Kurata M, Okuda Y, et al. Totally laparoscopic hepatectomy exposing the vessels around the tumor intended to secure the surgical margin. Surg Endosc 2014;28:1331-2. [Crossref] [PubMed]
- Honda G, Kurata M, Okuda Y, et al. Totally laparoscopic hepatectomy exposing the major vessels. J Hepatobiliary Pancreat Sci 2013;20:435-40. [Crossref] [PubMed]
- Ciria R, Berardi G, Nishino H, et al. A snapshot of the 2020 conception of anatomic liver resections and their applicability on minimally invasive liver surgery. A preparatory survey for the Expert Consensus Meeting on Precision Anatomy for Minimally Invasive HBP Surgery. J Hepatobiliary Pancreat Sci 2022;29:41-50. [Crossref] [PubMed]
Cite this article as: Ciria R, Ayllón MD, Briceño J. Liver gates to access everywhere in the liver: how can we learn? Dig Med Res 2023;6:28.


