
Narrative review of esophageal motility changes after endoscopic therapy for gastroesophageal reflux disease
Introduction
Gastroesophageal reflux disease (GERD) surgical treatment has survived 65 years—since Rudolph Nissen described his and the first fundoplication in 1956 (1)—despite several downfalls along time (2). Surgery has been accused of being not durable (3), carrying a high risk of mortality (4) (0.05% according to the authors of this review!), being morbid (5) and now of making too many holes in the abdomen. Thus, endoscopic therapy for GERD flourished (6). Innumerous and ingenious devices and techniques were created to decrease the complacency of the esophagogastric junction (creating bulking effect by injecting polymers, hydrogel or microbeads or inducing fibrosis by radiofrequency or, mucosectomy) or recreate a valve with an endofundoplication.
Studies on these alternatives to laparoscopic antireflux surgery should analyze the consequences on the esophageal motility that could shed light in the real usefulness of the method and the expectations for long term outcomes not focus only on short-term GERD control and morbidity. We opted to compile the motility changes after these procedures as there are plenty of other reviews on the techniques per se, outcomes and complications. As far as we know there are no narrative reviews on the motility showing results based on GERD pathophysiology.
This review is focused on the changes in esophageal motility after endoscopic therapy for GERD.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://dx.doi.org/10.21037/dmr-21-54).
Methods
The study is a narrative overview of the literature synthesizing the findings of literature retrieved. Data was retrieved from searching the computerized database PubMed for original and review papers on studies including manometry analysis of the esophageal motility after endoscopic therapy for GERD (injectable agents, mucosectomy, radiofrequency, endofundoplication). Additional hand searches were also performed.
Term used for search were ““Gastric Acid Reflux,” or ‘Esophageal Acid reflux “Gastroesophageal Reflux Disease,” or “GERD” AND “Endoscopic treatment,” or “Gastrointestinal Endoscopy,” or “Surgical Procedures,” or “Gastrointestinal Surgeries” AND “manometry”, or “motility”.
Three independent authors searched for papers.
Pathophysiology of GERD and how an antireflux procedure should work
We need to understand GERD pathophysiology and what is expected from an antireflux procedure to be successful before analyzing changes in esophageal motility.
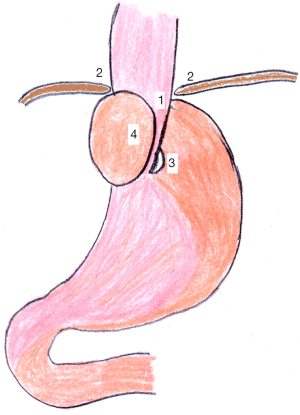
GERD pathophysiology is complex (7). Basically, a transdiaphragmatic pressure gradient (negative thoracic pressure and positive abdominal pressure) must be counteracted by a valve mechanism represented by the natural antireflux structures: (I) intra-abdominal length of the esophagus, (II) diaphragmatic sphincter, (III) angle of His, (IV) Gubaroff valves, and (V) lower esophageal sphincter (LES) (8) (Figure 1). Failure of a single component of this valval complex may not be enough to cause GERD. Thus, a hypotonic LES does not translate necessary into GERD (9). In fact, most natural antireflux structures are flaw in the setting of hiatal hernia but, again, the presence of a hiatal hernia is not synonym to GERD (10).

A hiatoplasty and fundoplication, the procedure to which others should be compared, is able to restore all mentioned natural antireflux structures (Figure 2) (11). The intra-abdominal length of the esophagus is restored if a hiatal hernia was present, the diaphragmatic hiatus is reapproximated, the angle of His is hyperaccentuated, and the LES is reinforced by the synergistic contractions of the gastric fundus. Similarly, in the presence of GERD, the correction of a single mechanism may not guarantee GERD control (12). Historically, every attempt to restore a single mechanism failed (12). Thus, an ideal antireflux procedure should be able to restore all natural antireflux structures.
Endoscopic GERD therapy: procedures to decrease the complacency of the esophagogastric junction
Injectable agents
The idea of injecting bulking agents to provide augmentation of the LES pressure started in 1984 when O’Connor and colleagues used both biodegradable and non-degradable material in dogs (13).
Copolymers
An injectable non-resorbable solution of 8% ethylene vinyl alcohol copolymer dissolved in dimethyl sulfoxide was used to treat patients with GERD for the first time in 1999 after previous studies in porcine models (13).
The procedure is performed as an outpatient procedure (13). The non-viscous solution is injected through a sclerotherapy-type needle near the squamocolumnar junction (Z-line), and 1–2 mL implant solution is injected deep into the wall circumferentially with fluoroscopy guidance (14).
In a multicenter prospective trial (15), 80% of the patients presented improvement in symptom scores, and cessation of proton pump inhibitors (PPI) was achieved in 86% at 12-month follow-up. pH normalization was achieved in only 39% of patients, and esophageal manometry revealed no significant change in the LES pressure or length, residual LES pressure, or in peristaltic amplitude. The same group of authors of mentioned above expanded the follow-up and published the data after 24 months of the procedure (16). Symptom scores remained stable after implantation. There was a decrease in the rate of patients off PPI from 86% to 67%. And there was not changes on previously described results of pH monitoring or esophageal manometry.
There are some cases of serious complications related to the use of this product (17) forcing removal from market due to safety concerns and lack of long-term efficacy (18).
Graphites
Graphite was approved by Food and Drug Administration (FDA) in 1999 to be initially used for the treatment of stress urinary incontinence and later in some cases of fecal incontinence (18). It was tested in a pilot study of 10 patients with moderate GERD published in 2009 (6).
It is composed of coated graphite beads containing zirconium oxide, suspended in a water-based, absorbable polysaccharide carrier gel (6). It is prepackaged in syringes containing 1.0 mL of the substance with a 20-gauge needle sclerotherapy catheter. The application is quite similar to the agent mentioned before. The substance is injected into the submucosal space in the region of the gastroesophageal junction (GEJ), at or within the z-line, in 4 quadrant injections (18).
In the pilot study mentioned before, all 10 patients were on daily PPI therapy and had a hiatal hernia (HH) <3 cm. Seven patients did not have erosive esophagitis and 3 patients had mild erosive esophagitis. In the follow-up of 12 months, there was an improvement of 90% in symptom scores; 70% of the patients were off all antacid medication and 90% reduced PPI use by greater than 50%. A manometric study of these patients was conducted before application but not described after the application and no other study showed changes in motility after this procedure.
This product is not currently FDA-approved for the treatment of GERD (6).
Hydrogel prosthesis
Hydrogel was initially tested in farm-pigs (19) and subsequently in patients with GERD for the first time at the end of 2000 (19,20).
The device is a 6-mm × 15-mm cylinder-shaped soft pliable cushion hydrogel prosthesis implanted into the submucosa of the GEJ (6). The hydrogel expands in 24 hours creating a mechanical anti-reflux barrier (20).
In a prospective randomized trial, 78 patients showed significant improvement in heartburn, regurgitation, and medication usage at 6 months. There was an improvement in the DeMeester score values, but without normalization in the follow-up. There was no statistically significant improvement in LES pressure compared with baseline (21). It was terminated early due to the lack of compelling efficacy data. In another European multicenter study (21,22), 79% of the patients had an improvement in symptom scores and 53% were off PPI use. At 6 months, 40% had a normal pH level. LES pressure went from 8.8 on baseline to 13.8 (P<0.01). This product was removed from the market because of poor long-term results (6,22).
Mucosectomy and band ligation
Anti-reflux mucosectomy (ARMS) was adopted as an alternative endoscopic method for GERD treatment after incidentally discovered in 2003 when a patient with Barret’s esophagus was submitted to endoscopic mucosal resection (EMR) and experienced improvement in GERD symptoms (23). As the mucosectomy area heals and scars, the tissue contracts to augment the natural antireflux valve.
It is considered one technique that does not require specialized equipment, and consists of a hemi-circumferential EMR of the gastric cardia around the GEJ. With the scope in a retroflexed position, the mucosa is marked with the snare 240–270º around de gastroesophageal valve. Then the mucosa of the cardia is raised with solutions, and then the tissue is banded and transected with forced coagulation (6,23).
In the largest series of ARMS conducted by Yoo et al. and encompassing 33 patients, 63% of patients completely discontinued PPI, and there was a significant reduction in GERD health-related quality of life (HRQL) scores. There was an increase of the LES pressure from 16.3 to 20.7 at 6 months (P=0.005) (24).
With the same mechanism to augment the natural antireflux valve mentioned before, and as another alternative method, some authors perform the clip band ligation anti-reflux therapy. Using a multi-band device, two bands were ligated to the cardial mucosa and fixed with a single-use clip. Promoting the protrusion of the cardial tissue, the space is reduced by constricting the anterior and posterior walls of the cardia with two clips at the 6 and 12 o’clock positions (25). Using this technique, the DeMeester score decreased from 105.9±74.8 to 41±43.8, HRQL showed a significant improvement 6 months later the procedure, and 43% of the patients discontinued PPIs. There was no significant improvement on LES pressure compared to baseline 6 and 12 months after (25,26).
Radiofrequency (RF)
RF energy may be applied to the distal esophagus, GEJ, and the cardia (6,27). The first series reported with the use of this method was published in 2000 in canine and porcine models (27). It is performed transorally initially with a conventional endoscopy, then the distance from the incisors to the z-line is measured, and the endoscope removed. A flexible RF energy catheter is passed transorally and positioned 2cm distal to the level of z-line. Low-power RF energy is delivered to the deeper muscular layers of the esophagus and stomach, leading to augmentation of the LES and increasing resistance to reflux during gastric distension.
In a multicenter prospective study with 118 patients treated with RF, there were improvements in symptoms with reduction of heartburn and GERD HRQL scores at 12 months. 61% of the patients discontinued PPI use or used over-the-counter. The DeMeester score improved from 40.0 to 26.3 (28). Only 18 of the patients were submitted to esophageal manometry that showed reduction in the number of transient LES relaxations, but without significant change in other esophageal motility parameters (29). In a double-blind sham-controlled study from Belgium, patients submitted to radiofrequency treatment of the GEJ presented improvement in symptom scores, but no changes were observed in esophageal acid exposure and LES pressure. (30)
A systematic review and meta-analysis revealed an improvement of 65% in symptom scores, and 75–86% of patients were medication free at follow-up. This procedure was able to reduce but not to normalize esophageal acid exposure or DeMeester scores in pH monitoring results. There was not significant change in LES pressure after the radiofrequency procedure. The rate of failure of the radiofrequency delivery to GEJ was almost 60%, and these patients required an anti-reflux surgery 6 months after the endoscopic procedure for GERD treatment (31).
Endoscopic GERD therapy: endofundoplication
Also called transoral incisionless fundoplication (TIF), endofundoplication was first described in 1992 using an endoscopic transgastric approach in pigs (32). Currently, the procedure consists in creating a 3.0 cm in length and 200° to 300° circumference valve, through a full-thickness plication of distal esophagus and cardia using a single use device guided by endoscopic retroflexion view. TIF operates trying to rebuild the anatomy of gastric cardia and strengthening a valve mechanism. (33)
Summarizing the results of many studies, short term follow-up showed improvement in symptom scores; 40–90% of patients stopped using PPI at some stage of follow-up, and 40–80% had normalization of esophageal pH monitoring (34). In the opposite side, in a 6 years’ follow-up, the rate of PPI-free patients reduced to about 30%. (35).
Regarding esophageal motility, Rinsma et al. (36) demonstrated in a follow-up of 6 months after TIF that there was a reduction in the number of postprandial transient LES relaxations (TLESRs), as well as in the TLESRs associated with reflux. Otherwise, Schwartz et al. (37) and Testoni et al. (35,38) showed no significant changes in LES basal pressure or distal esophageal amplitude (DEA) in a 12-month follow-up. Some papers propose that the improvement of the symptoms occurred due to the creation of greater length new valve more than the increasement of the valve pressure (35,38).
Bell et al. founded normalization of acid exposure and DeMeester score in 61% and 56% of the patients, respectively, in a 6-months follow-up (39). On the other hand, other studies demonstrated a reduction on acid exposure but not reaching normal values of physiologic acid exposure (35,40,41).
When we analysis morphological assessment, Kalapala et al. demonstrated in a 12-months follow-up that new valve Hill grade I was presented in 77.8% of the patients (41). After 24 months, Testoni et al. showed that in 50% of the patients there is a recurrence of the hiatal hernia, and in patients with Hill grade of the gastroesophageal valve II or III before the TIF, the new valve Hill grade I was presented in 63.7% and 33.6% respectively (35,41).
Discussion
This review focused on the changes in esophageal motility after endoscopic therapy for GERD (injectable agents, mucosectomy, radiofrequency, endofundoplication). Several ingenious devices and techniques were created but, unfortunately, often ignoring lessons learned from the past (12). Previous experiences to treat GERD restoring a single antirreflux mechanism failed. The consequences of a recurrent hiatal hernia after a fundoplication are well-known (42). Symptoms reappear even though the LES is reinforced with a fundoplication. Similarly, LES augmentation with a magnetic ring around the GEJ brings suboptimal GERD control since the angle of His is not hyperaccentuated (43). Available and past endoscopic techniques focused essentially on the augmentation of the LES. Some endoscopic techniques rely on devices implanted at the GEJ. Again, history showed that foreign body around a mobile viscus may be catastrophic leading to complications and a high rate of removal. This was true for the Angelchik prosthesis (44) and now to the magnetic ring (43). Not surprisingly, several devices were removed from market due to complications or poor outcomes.
Most studies that we reviewed evaluate subjective outcomes, rarely through esophageal function tests. Also, the methodology quality of the studies is not always ideal. There are few prospective studies, no studies with a significant number of individuals and, curiously, most papers dealing with a specific technique comes from the same groups. There is scarce data on injectable agents and most were discontinued in the market due to complications. Mucosectomy and band ligation are new methods with few studies yet. Most data available comes from studies based on radiofrequency and endofundoplication. Although some techniques may increase lower esophageal sphincter basal pressure, GERD control is generally suboptimal with decrease in acid exposure time but not normalization to physiologic values (Table 1). Future technology must consider GERD pathophysiology. Endofundoplication seems to be the most promising endoscopic technique. The development of new images methods adapted to the endoscope may allow an endoscopic hiatal repair in the future. The current alternative of performing a laparoscopic hiatal repair combined to endofundoplication (45) seems like an illogic overindication of the endoscopic method.
Table 1
| Outcomes/technique | Copolymers | Graphites | Hydrogel prothesis | Mucosectomy | Radiofrequency | Endofundoplication |
|---|---|---|---|---|---|---|
| Symptom scores improvement | 80% | 90% | 80% | 70% | 65% | 40% |
| Off PPI’s | 65% | 70% | 50% | 60% | 80% | 65% |
| DeMeester normalization | No | No | No | No | No | No |
| pH normalization | 40% | 40% | 40% | - | - | 60% |
| LESP improvement | N/S | N/S | Yes | N/S | N/S | N/S |
| tLESr improvement | N/S | N/S | N/S | N/S | N/S | N/S |
PPI, proton pump inhibitors; LESP, lower esophageal sphincter pressure; tLESr, transient lower esophageal sphincter relaxations; N/S, not studied.
Laparoscopic fundoplication and hiatoplasty brings excellent and durable symptomatic as well as manometric and pHmetric outcomes even after 15 years (44, 46). Any new technology or operation must be compared to these results. Current endoscopic therapy modalities certainly did not reach these outcomes yet.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://dx.doi.org/10.21037/dmr-21-54
Peer Review File: Available at https://dx.doi.org/10.21037/dmr-21-54
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/dmr-21-54). MGP serves as an unpaid editorial board member of Digestive Medicine Research from Jun. 2021 to May 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Herbella FA, Matone J, Del Grande JC. Eponyms in esophageal surgery, part 2. Dis Esophagus 2005;18:4-16. [Crossref] [PubMed]
- Wang YR, Dempsey DT, Richter JE. Trends and perioperative outcomes of inpatient antireflux surgery in the United States, 1993-2006. Dis Esophagus 2011;24:215-23. [Crossref] [PubMed]
- Spechler SJ, Lee E, Ahnen D, et al. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA 2001;285:2331-8. [Crossref] [PubMed]
- Bredenoord AJ, Pandolfino JE, Smout AJ. Gastro-oesophageal reflux disease. Lancet 2013;381:1933-42. [Crossref] [PubMed]
- Maret-Ouda J, Markar SR, Lagergren J. Gastroesophageal Reflux Disease: A Review. JAMA 2020;324:2536-47. [Crossref] [PubMed]
- Kushner BS, Awad MM, Mikami DJ, et al. Endoscopic treatments for GERD. Ann N Y Acad Sci 2020;1482:121-9. [Crossref] [PubMed]
- Herbella FA, Patti MG. Gastroesophageal reflux disease: From pathophysiology to treatment. World J Gastroenterol 2010;16:3745-9. [Crossref] [PubMed]
- Menezes MA, Herbella FAM. Pathophysiology of Gastroesophageal Reflux Disease. World J Surg 2017;41:1666-71. [Crossref] [PubMed]
- Benatti CD, Herbella FA, Patti MG. Manometric parameters in patients with suspected Gastroesophageal reflux disease and normal pH monitoring. Gastroenterol Endosc Dig 2014;33:52-7.
- Schlottmann F, Andolfi C, Herbella FA, et al. GERD: Presence and Size of Hiatal Hernia Influence Clinical Presentation, Esophageal Function, Reflux Profile, and Degree of Mucosal Injury. Am Surg 2018;84:978-82. [Crossref] [PubMed]
- Herbella FAM, Schlottmann F, Patti MG. Pathophysiology of gastroesophageal reflux disease: how an antireflux procedure works (or does not work). Updates Surg 2018;70:343-7. [Crossref] [PubMed]
- Chang KJ. Endoscopic foregut surgery and interventions: The future is now. The state-of-the-art and my personal journey. World J Gastroenterol 2019;25:1-41. [Crossref] [PubMed]
- Louis H, Closset J, Devière J. Enteryx. Best Pract Res Clin Gastroenterol 2004;18:49-59. [Crossref] [PubMed]
- Johnson DA. Enteryx for gastroesophageal reflux disease. Expert Rev Med Devices 2005;2:19-26. [Crossref] [PubMed]
- Johnson DA, Ganz R, Aisenberg J, et al. Endoscopic implantation of enteryx for treatment of GERD: 12-month results of a prospective, multicenter trial. Am J Gastroenterol 2003;98:1921-30. [Crossref] [PubMed]
- Cohen LB, Johnson DA, Ganz RA, et al. Enteryx implantation for GERD: expanded multicenter trial results and interim postapproval follow-up to 24 months. Gastrointest Endosc 2005;61:650-8. [Crossref] [PubMed]
- Wong RF, Davis TV, Peterson KA. Complications involving the mediastinum after injection of Enteryx for GERD. Gastrointest Endosc 2005;61:753-6. [Crossref] [PubMed]
- Ganz RA, Fallon E, Wittchow T, et al. A new injectable agent for the treatment of GERD: results of the Durasphere pilot trial. Gastrointest Endosc 2009;69:318-23. [Crossref] [PubMed]
- Easter DW, Yurek M, Summers H, et al. Endoscopic prosthesis augmentation of the lower esophageal sphincter in swine. Am J Surg 2001;182:697-701. [Crossref] [PubMed]
- Fockens P. Gatekeeper Reflux Repair System: technique, pre-clinical, and clinical experience. Gastrointest Endosc Clin N Am 2003;13:179-89. [Crossref] [PubMed]
- Fockens P, Cohen L, Edmundowicz SA, et al. Prospective randomized controlled trial of an injectable esophageal prosthesis versus a sham procedure for endoscopic treatment of gastroesophageal reflux disease. Surg Endosc 2010;24:1387-97. [Crossref] [PubMed]
- Fockens P, Bruno MJ, Gabbrielli A, et al. Endoscopic augmentation of the lower esophageal sphincter for the treatment of gastroesophageal reflux disease: multicenter study of the Gatekeeper Reflux Repair System. Endoscopy 2004;36:682-9. [Crossref] [PubMed]
- Hedberg HM, Kuchta K, Ujiki MB. First Experience with Banded Anti-reflux Mucosectomy (ARMS) for GERD: Feasibility, Safety, and Technique (with Video). J Gastrointest Surg 2019;23:1274-8. [Crossref] [PubMed]
- Yoo IK, Ko WJ, Kim HS, et al. Anti-reflux mucosectomy using a cap-assisted endoscopic mucosal resection method for refractory gastroesophageal disease: a prospective feasibility study. Surg Endosc 2020;34:1124-31. [Crossref] [PubMed]
- Liu S, Chai N, Zhai Y, et al. New treatment method for refractory gastroesophageal reflux disease (GERD): C-BLART (clip band ligation anti-reflux therapy)-a short-term study. Surg Endosc 2020;34:4516-24. [Crossref] [PubMed]
- Hu HQ, Li HK, Xiong Y, et al. Peroral endoscopic cardial constriction in gastroesophageal reflux disease. Medicine (Baltimore) 2018;97:e0169 [Crossref] [PubMed]
- Triadafilopoulos G, Dibaise JK, Nostrant TT, et al. Radiofrequency energy delivery to the gastroesophageal junction for the treatment of GERD. Gastrointest Endosc 2001;53:407-15. [Crossref] [PubMed]
- Triadafilopoulos G, DiBaise JK, Nostrant TT, et al. The Stretta procedure for the treatment of GERD: 6 and 12 month follow-up of the U.S. open label trial. Gastrointest Endosc 2002;55:149-56. [Crossref] [PubMed]
- Sowa P, Samarasena JB. Nonablative Radiofrequency Treatment for Gastroesophageal Reflux Disease (STRETTA). Gastrointest Endosc Clin N Am 2020;30:253-65. [Crossref] [PubMed]
- Arts J, Bisschops R, Blondeau K, et al. A double-blind sham-controlled study of the effect of radiofrequency energy on symptoms and distensibility of the gastro-esophageal junction in GERD. Am J Gastroenterol 2012;107:222-30. [Crossref] [PubMed]
- Perry KA, Banerjee A, Melvin WS. Radiofrequency energy delivery to the lower esophageal sphincter reduces esophageal acid exposure and improves GERD symptoms: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech 2012;22:283-8. [Crossref] [PubMed]
- Jennings RW, Flake AW, Mussan G, et al. A novel endoscopic transgastric fundoplication procedure for gastroesophageal reflux: an initial animal evaluation. J Laparoendosc Surg 1992;2:207-13. [Crossref] [PubMed]
- Chang KJ, Bell R. Transoral Incisionless Fundoplication. Gastrointest Endosc Clin N Am 2020;30:267-89. [Crossref] [PubMed]
- Bazerbachi F, Krishnan K, Abu Dayyeh BK. Endoscopic GERD therapy: a primer for the transoral incisionless fundoplication procedure. Gastrointest Endosc 2019;90:370-83. [Crossref] [PubMed]
- Testoni PA, Testoni S, Mazzoleni G, et al. Long-term efficacy of transoral incisionless fundoplication with Esophyx (Tif 2.0) and factors affecting outcomes in GERD patients followed for up to 6 years: a prospective single-center study. Surg Endosc 2015;29:2770-80. [Crossref] [PubMed]
- Rinsma NF, Smeets FG, Bruls DW, et al. Effect of transoral incisionless fundoplication on reflux mechanisms. Surg Endosc 2014;28:941-9. [Crossref] [PubMed]
- Schwartz MP, Wellink H, Gooszen HG, et al. Endoscopic gastroplication for the treatment of gastro-oesophageal reflux disease: a randomised, sham-controlled trial. Gut 2007;56:20-8. [Crossref] [PubMed]
- Testoni PA, Testoni S, Mazzoleni G, et al. Transoral incisionless fundoplication with an ultrasonic surgical endostapler for the treatment of gastroesophageal reflux disease: 12-month outcomes. Endoscopy 2020;52:469-73. [Crossref] [PubMed]
- Bell RC, Freeman KD. Clinical and pH-metric outcomes of transoral esophagogastric fundoplication for the treatment of gastroesophageal reflux disease. Surg Endosc 2011;25:1975-84. [Crossref] [PubMed]
- Hunter JG, Kahrilas PJ, Bell RC, et al. Efficacy of transoral fundoplication vs omeprazole for treatment of regurgitation in a randomized controlled trial. Gastroenterology 2015;148:324-333.e5. [Crossref] [PubMed]
- Kalapala R, Karyampudi A, Nabi Z, et al. Endoscopic full-thickness plication for the treatment of PPI-dependent GERD: results from a randomised, sham controlled trial. Gut 2021; Epub ahead of print. [Crossref] [PubMed]
- Schlottmann F, Laxague F, Angeramo CA, et al. Outcomes of Laparoscopic Redo Fundoplication in Patients With Failed Antireflux Surgery: A Systematic Review and Meta-analysis. Ann Surg 2021;274:78-85. [Crossref] [PubMed]
- DeMarchi J, Schwiers M, Soberman M, Tokarski A. Evolution of a novel technology for gastroesophageal reflux disease: a safety perspective of magnetic sphincter augmentation. Dis Esophagus 2021; Epub ahead of print. [Crossref] [PubMed]
- Varshney S, Kelly JJ, Branagan G, et al. Angelchik prosthesis revisited. World J Surg 2002;26:129-33. [Crossref] [PubMed]
- Nguyen NT, Chinn J, Chang K. Collaboration between GI surgery & Gastroenterology improves understanding of the optimal antireflux valve-the omega flap valve. Surg Endosc 2021;35:3214-20. [Crossref] [PubMed]
- Csendes A, Orellana O, Cuneo N, et al. Long-term (15-year) objective evaluation of 150 patients after laparoscopic Nissen fundoplication. Surgery 2019;166:886-94. [Crossref] [PubMed]
Cite this article as: de Padua F, Centeno DM, Herbella FAM, Patti MG. Narrative review of esophageal motility changes after endoscopic therapy for gastroesophageal reflux disease. Dig Med Res 2021;4:51.


