Endoscopic recanalization using rendez-vous technique for complete upper esophageal obstruction: a case report
Introduction
Complete esophageal obstruction is a rare adverse effect after head and neck radiotherapy, with an incidence of 0.8% for the patients with a radiation exposure over 60 Gy (1-4). Other etiologies include the ingestion of caustic substances with subsequent inflammation, fibrosis and collagen deposition in the esophagus (5). With severe clinical symptoms of aphagia and multiple aspirations, complete obstruction significantly affects one’s quality of life. Indeed, patients can no longer swallow their saliva and a feeding gastrostomy becomes necessary for nutritional support (6).
The management of these lesions is technically challenging and the approach to complete esophageal obstruction is not well established in cases where malignant recurrence has been ruled out. Historically, surgery was the only treatment option, with significant mortality and morbidity. More recently, endoscopic techniques are now proposed to restore luminal patency. We hereby describe an endoscopic rendez-vous technique for complete upper esophageal obstruction in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/dmr-20-154).
Case presentation
A 69-year-old patient, with past medical history of inflammatory bowel disease, developed a complete upper esophageal stenosis, 6 months after radiochemotherapy treatment for a left hypopharyngeal epidermoid cancer with proximal esophageal extension. The patient presented with total dysphagia, significant weight loss and multiple aspiration episodes. A complete upper esophageal obstruction, just distal to the upper esophageal sphincter, was confirmed by upper endoscopy and a barium study. A neoplastic recurrence was ruled out. The benefits and the risks of the endoscopic and the surgical management were weighted and the endoscopic rendez-vous technique was chosen (Video 1).
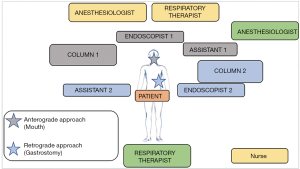
The rendez-vous endoscopic technique requires a complex set-up as well as a team-work approach (Figure 1). As pictured, there should be enough space for the anesthesiologist, the respiratory therapist and the radiology technologist with the fluoroscopy C-arm. Two interventional endoscopists with their assistants and their columns are positioned for an antegrade approach through the mouth and a retrograde approach through the gastrostomy. Importantly, similarly to other third-space endoscopy procedures, the use of CO2 is mandatory. The intervention is performed supine under general anesthesia. Prophylactic antibiotics are given at the beginning of the procedure.
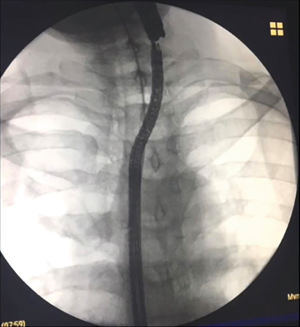
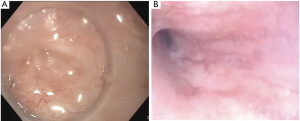
The first step is to locate the obstruction by the antegrade approach with an adult gastroscope (Figure 2A) and by the retrograde approach with a pediatric gastroscope (Figure 2B). Once the two scopes are fluoroscopically aligned, a transillumination is performed. Subsequently, using fluoroscopy, the length of the stenosis is measured (Figure 3).
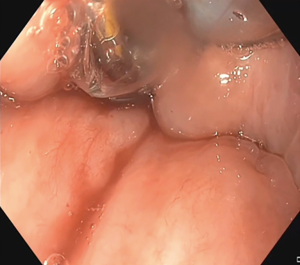
The second step is the puncture and dissection of the fibrotic mucous membrane by antegrade approach with the needle knife, after perfect alignment of the two gastroscopes, under endoscopic and fluoroscopic control. Passage of a guidewire from the oral side is used for lumen restoration (Figure 4). Alignment of the two gastroscopes is essential to avoid muscular wall injury. The guidewire is then externalized on one side through the gastrostomy opening and on the other side through the mouth (Figure 5). In cases where the stenosis is right at the upper esophageal sphincter, alignment of the two gastroscopes can be unstable while advancing the guidewire. Use of a transparent straight endoscopic cap may be useful as it improves visualization and tissue traction (Figure 4).
The third step is the balloon dilatation (Figure 6). The fluoroscopic view is particularly useful to ensure adequate placement of the balloon across the stenosis. The absence of perforation on the recanalization path must be carefully checked following the dilatation with passage of the smaller gastroscope. Alternatively, lack of contrast extravasation effectively rules out significant muscular injury.
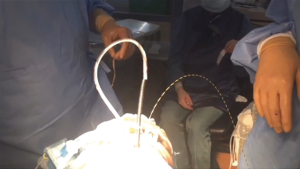
Following the successive dilatations, a nasogastric (NG) tube is inserted to prevent early recurrence of the stenosis. Further balloon dilatations might be necessary to successfully insert the NG tube. Another alternative technique in case of unsuccessful attempts is to advance the pediatric gastroscope by the retrograde approach through the stenosis and to externalize it through the mouth (Figure 7). The NG tube is then taped to the end of the pediatric gastroscope. The scope can then be pulled back through the gastrostomy site and the NG tube successfully pushed back in the stomach.
Further serial dilatations after the discharge are usually necessary to obtain a satisfying functional result. Depending on the clinical evolution, these dilatations can be progressively spaced-out. Close speech therapy follow-up is also required after the procedure.
Follow-up with both barium studies and upper endoscopy is optimal. In our case, a dilatation was planned on post-operative day 2 and the patient was discharged the following day. Subsequent dilatations were necessary to obtain a satisfying functional result. These dilatations were initially performed under general anesthesia to ensure easier cannulation of the stenotic lumen. Initially, they were performed every 1–2 weeks, and they were progressively spaced-out. A laser debridement with the ENT team was also performed. A barium study performed 6 months post recanalization shows a quick passage of contrast through the previous stenotic area (Figure 8). At 10-month follow-up, the patient had a dilatation once every 2 months. He was still undergoing speech therapy and is now tolerating a semi-solid diet. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient.
Comments
We hereby present the management of complete esophageal obstruction by an endoscopic rendez-vous technique, which is a good minimally invasive approach for these difficult clinical problems.
Historically, surgery was the only treatment option, with significant mortality and morbidity (7). The surgical options include colonic interposition or jejunal graft for esophageal replacement after the surgical resection of the stenotic portion of the esophagus (3). However, these options are more invasive and not privileged with upper esophageal obstructions. Furthermore, previous use of radiotherapy makes surgical interventions even more challenging.
Hence, multiple minimally invasive therapeutic managements are now proposed to restore luminal patency. Endoscopic alternatives include balloon or bougie dilatation as well as stenting if the stenosis is incomplete. The main risk associated with these techniques is esophageal perforation (6). In the case of total esophageal obstruction with no visible hiatus, another alternative is the retrograde puncture of the stenotic lesion with laryngoscopic guidance and utilization of tactile impression for recanalization (8). However, this technique may not be appropriate for fibrous obstructions.
Recanalization using the rendez-vous technique after transillumination has recently become the most popular endoscopic approach for complete obstructions. Studies suggest that this technique is safe and reliable (9). Fusco et al. reported a series of 19 patients who underwent recanalization by endoscopic rendez-vous technique with a success rate of 94.7%. However, previous studies suggest that strictures length superior to 3 cm and absence of transillumination are factors associated with adverse outcomes with the rendez-vous technique (1). In the absence of transillumination, an alternative is to perform a submucosal tunneling to allow for a passage across the stenosis then followed by dilatation. This technique may be associated with minor cutaneous emphysema and capnomediastinum (10). For example, the Peroral Endoscopic Tunneling for Restoration of the Esophagus (POETRE) technique uses this submucosal tunneling approach (11).
The main adverse outcome of the endoscopic rendez-vous technique is a perforation towards the upper airways. The presence of a pneumomediastinum is not a reliable sign of perforation as the procedure may require prolonged CO2 insufflation and the esophagus does not have a serous membrane. The management of true perforations include stenting, through-the-scope or over-the-scope clips, endoscopic suturing, endoscopic vacuum therapy or in cases of endoscopic failure direct surgical approach. In a large serie, no cases of perforation or mediastinitis were reported for the 19 patients who underwent the procedure (9). In another case-serie, two patients out of eight had evidence of esophageal microperforation after their procedure. Only one of these two patients had clinical subcutaneous emphysema and no subsequent treatments were necessary (6). Other studies report three cases of perforation in 35 procedures, with one of them necessitating an esophageal stent and the two others treated conservatively. One case of self-limited hematemesis in 35 procedures was also reported (1).
One of the goals of this management would be to remove the feeding gastrostomy after the procedure. In Fusco series, only 3 patients out of 19 had their gastrostomy removed (9). In other studies, only 8 of 44 patientshad their gastrostomy eventually removed after the procedure (1). However, it was not possible to determine if these gastrostomies were kept because of persistent dysphagia or prophylactically. Furthermore, in most cases, the rendez-vous technique requires a long-term follow-up with regular dilatations. In Fusco’s series, patients required a mean 11 follow-up dilatations or bouginages during a 2.2-year mean follow-up (9). Auto-bouginages, when possible, can improve the patients’ quality of life. Importantly, a team approach bringing together the interventional endoscopist, head and neck and thoracic surgeon, radiation oncologist, speech therapist and dietician is essential for the long-term success of these procedures. This multidisciplinary team is required to manage the complex medical needs of these patients.
Technical success of recanalization is defined as the restoration of esophageal continuity and the ability to pass the scope through the stenosis. Clinical success is defined as an improvement in the dysphagia score (3). However, there is a discrepancy between technical and clinical success since dysphagia is not only related to the mechanical obstruction, but also to the damage to the nerves and the muscles involved with the radiotherapy (9). Although the rendez-vous approach does not provide total recovery of the esophageal function in most patients, it offers good functional results, and it may significantly improve the patient’s quality of life.
Some strengths and limitations of this study should be mentioned. The patient was closely followed with clinical assessment, endoscopic examination and radiologic studies after the surgery. However, the relatively short follow-up time in this case does not provide information about the long-term results of these endoscopic recanalization procedures.
Summary
Complete upper esophageal obstruction is a clinical challenge and the approach to these obstructions is not well established. The endoscopic rendez-vous technique is a reliable and safe therapeutic option for short stenosis with transillumination. Although the technical success rate appears to be quite high, clinical success may be variable. A multidisciplinary approach and long-term follow-up is mandatory in order to maximize the functional benefit for these complex patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/dmr-20-154
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-154). Dr. GR reports personal fees from Medtronic, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Grooteman KV, Wong Kee Song LM, Vleggaar FP, et al. Functional outcome of patients treated for radiation-induced complete esophageal obstruction after successful endoscopic recanalization (with video). Gastrointest Endosc 2014;80:175-81. [Crossref] [PubMed]
- Lawson JD, Otto K, Grist W, et al. Frequency of esophageal stenosis after simultaneous modulated accelerated radiation therapy and chemotherapy for head and neck cancer. Am J Otolaryngol 2008;29:13-9. [Crossref] [PubMed]
- Perbtani Y, Suarez AL, Wagh MS. Emerging techniques and efficacy of endoscopic esophageal reconstruction and lumen restoration for complete esophageal obstruction. Endosc Int Open 2016;4:E136-42. [Crossref] [PubMed]
- Zackrisson B, Mercke C, Strander H, et al. A systematic overview of radiation therapy effects in head and neck cancer. Acta Oncol 2003;42:443-61. [Crossref] [PubMed]
- Cheng HT, Cheng CL, Lin CH, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol 2008;8:31. [Crossref] [PubMed]
- Maple JT, Petersen BT, Baron TH, et al. Endoscopic management of radiation-induced complete upper esophageal obstruction with an antegrade-retrograde rendezvous technique. Gastrointest Endosc 2006;64:822-8. [Crossref] [PubMed]
- Zhou JH, Jiang YG, Wang RW, et al. Management of corrosive esophageal burns in 149 cases. J Thorac Cardiovasc Surg 2005;130:449-55. [Crossref] [PubMed]
- Lew RJ, Shah JN, Chalian A, et al. Technique of endoscopic retrograde puncture and dilatation of total esophageal stenosis in patients with radiation-induced strictures. Head Neck 2004;26:179-83. [Crossref] [PubMed]
- Fusco S, Kratt T, Gani C, et al. Rendezvous endoscopic recanalization for complete esophageal obstruction. Surg Endosc 2018;32:4256-62. [Crossref] [PubMed]
- Babich JP, Diehl DL, Entrup MH. Retrograde submucosal tunneling technique for management of complete esophageal obstruction. Surg Laparosc Endosc Percutan Tech 2012;22:e232-5. [Crossref] [PubMed]
- Wagh MS, Draganov PV. Per-oral endoscopic tunneling for restoration of the esophagus: a novel endoscopic submucosal dissection technique for therapy of complete esophageal obstruction. Gastrointest Endosc 2017;85:722-7. [Crossref] [PubMed]
Cite this article as: Alaoui AA, Studer AS, Rakovich G, Kaouam N, Ayad T, Atlas H, Garneau PY, Denis R, Pescarus R. Endoscopic recanalization using rendez-vous technique for complete upper esophageal obstruction: a case report. Dig Med Res 2021;4:2.