
Feasibility study of shortening the no drinking time before gastroscopy to two hours
Introduction
Gastroscopy is a useful and reliable method for detecting and diagnosing diseases and plays a crucial role in selecting clinical treatments. Patients usually feel uncomfortable during the examination, thus, intravenous sedation has been introduced to reduce patient anxiety during endoscopy (1). Among them, propofol sedation is applied for almost all complex endoscopic procedures and the majority of diagnostic upper and lower gastrointestinal endoscopies.
Although sedation improves the quality of the procedure and the patient reports better satisfaction, there are some potential risks, such as aspiration pneumonitis (2). To prevent aspiration pneumonia, patients are required to fast for a long time. But long-term fasting can cause thirst, anxiety, dehydration, hypoglycaemia, it may also increase the risk of postoperative nausea and vomiting (3,4). Moreover, large procedural sedation series (including one with 139,142 sedation events) have failed to identify any relationship between fasting and aspiration or other adverse events (5-7).
Before operating, no fluids or solid foods can patients take in a long time as the ASA guidelines suggests. That is because the stomach must be empty while operating. The guidelines point out that they should fast at least 2 hours after drinking water and 6 hours after having light meals before sedation. We need to consider the possibility of pulmonary aspiration of gastric contents when finding impaired gastric emptying or other emergency (I) ideal sedation level, (II) determination on delaying the procedure (III) determination on requiring endotracheal intubation to protect the airway (8).
There is no practice standard for pre-procedural fasting that has been universally accepted. The aim of this study is to explore how much water could we intake and feasibility of shortening the no drinking time before gastroscopy to two hours under procedural sedation. These data may contribute to a realistic judgement of relevant sedation associated complications during gastrointestinal endoscopy in clinical practice. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/dmr-20-64).
Methods
Materials
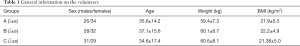
A total of 180 healthy volunteers participated in this experiment, gastroscopy was performed in The Seventh Affiliated Hospital, Sun Yat-sen University. The inclusion criteria were as follows: 18–69 years, without serious heart and lung diseases, ASA I-II. The exclusion criteria were as follows: patients with a history of abdominal surgery, obesity, suspected gastroesophageal reflux, pyloric obstruction, or intestinal obstruction and those who received medications that had effects on gastric secretion and empty within 24 hours prior to the experiment. The volunteers included 85 males and 95 females aged from 22 to 65 (Table 1).
Full table
Study methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the Seventh Affiliated Hospital of Sun Yat-sen University (No.: KY-2021-024-01). Informed consent was signed before 180 volunteers were examined. All member in three groups were fast for more than eight hours before the experiment. Members in group A drank 500 mL of water within 5 minutes, group B drank the maximum amount of water within 5 minutes, which was at least 500 mL. Group C, the control group, was not allowed to drink liquid for more than 8 hours. Abdominal doppler ultrasound (Aloka SSD 1700) was performed to measure the intragastric fluid volume every 15 minutes in groups A and B. Gastric emptying time was measured indirectly using two-dimensional ultrasound to measure the antral cross-sectional area (CSA), anteroposterior diameter (AP), gastric antrum left and right diameter (LL). Gastric antrum volume = AP+1/2 LL, until the antrum can be seen clearly under ultrasound. Gastroscopy (PENTAX, EG-29) was used to absorb the residual gastric liquid, which was measured by a test mixer. All gastroscopy is anesthetized with propofol. The completion rate and the incidence of aspiration were compared between the observation group and control group.
Statistical analysis
SPSS17.0 (SPSS, Chicago, Illinois, USA) was used to analyze the data, and ANOVA statistical method was performed. The measurement data are summarized as the x±s, and the enumeration data are summarized as the %. According to the χ2 test, P<0.05 was considered statistically significant.
Results
General information
There were no statistically significant differences in sex, age, weight or BMI in across the three groups (P>0.05).
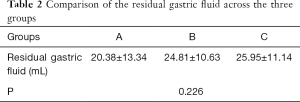
The comparison of the effects of drinking different amounts of water
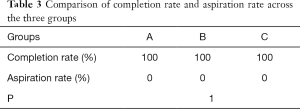
All members in group A drank 500 mL within 5 minutes; the emptying time ranged from 15–75 minutes, the average time was 39.81 minutes, the residual volume measured by gastroscopy ranged from 5–50 mL, and the average volume was 20.38 mL. In addition, group B drank 550–1,000 mL of water within 5 minutes; the average volume was 787.31±166.82 mL, the emptying time ranged from 15–75 minutes, the average emptying time was 40.38 minutes, the residual volume measured by gastroscopy ranged from 10–60 mL, and the average volume was 24.81 mL. The residual volume in control group C ranged from 0–60 mL, with an average of 25.95 mL (Tables 2-4). All volunteers in the three groups completed the experiments without aspiration, and the difference was not statistically significant (P>0.05).
Full table
Full table

Full table
Discussion
Pulmonary aspiration is a rare but potentially life-threatening complication of sedation, avoidance of which is the goal of preprocedural fasting guidelines. Fluid fasting policy advanced from the 1960s’ ‘nil by mouth’ dogma to more permissive international guidelines. In the advanced guidelines, adults are advised that in the 2 hours before operating, no fluid can be taken while for children, an hour is enough (9,10). This advice aims to recognize solids and liquids in gastric emptying.
Refraining from drinking liquid for a long time is not beneficial, and it is currently not guaranteed to be harmless. A survey from UK practice revealed that the comfort of patients undergoing general anaesthesia can be obviously decreased when starving for over 6 h, and over 2 h fluid fasting; 68% (131/193) of endoscopy departments perhaps enhances the discomfortable feeling significantly by excessive hanger; 68% (131/193) of units forbids patients to have clear fluid within 2 h of gastroscopy for the risk of significant aspiration in patients increases if he having fluids over 2 h who are now undergoing general anaesthesia (11). However, ignorance or unenforced with no problems recorded on preprocedural fasting take place in numerous sedation settings, including dentistry, therapeutic abortions, cardiac catheterization, echocardiography, and cataract surgery.
The aim of this clinical experiment was to explore the feasibility of shortening the no drinking time before gastroscopy to 2 hours. In our study, both the volunteers who drank 500 mL of water and those who drank the average amount of water 787 mL had emptied stomachs within 75 minutes, and there was no significant difference in the amount of residual liquid in the stomach between these volunteers and the control group (Table 4), who were not allowed to drink liquid for 8 hours. This experiment fully confirms that there is no correlation between fasting and the gastric fluid volume when the gastric emptying time is exceeded.
Before the concept of ERAS (enhanced recovery after surgery) was introduced to China, all patients undergoing gastrointestinal tract surgeries had to fast for more than 8 hours. Currently, ERAS has been implemented in China for more than 10 years. The clinical research and application results show that drinking 800 mL of clear water in 10 hours or 400 mL in 2 hours before surgery can reduce patient’s levels of thirst, hunger, annoyance or reduce insulin resistance after surgery, without increasing the risk of reflux and aspiration under anesthesia (12). For gastrointestinal tract surgeries, patients are allowed to drink 400 mL of clear water before surgery, and the effect of gastroscopy on the human body is lower than that of surgery, so it is safe to intake a certain amount of water before gastroscopy. In our study, all volunteers who consumed 500–1,000 mL water could empty their stomach within 75 minutes, and there was no significant difference between these volunteers and those who could not drink liquid for 8 hours. The evidence shows that if the amount water intake does not exceed 1,000 mL, the gastric emptying effect is equivalent. In our trial, all volunteers completed the gastroscopy examination, and no reflux or aspiration events occurred, which further confirms the safety of not drinking 2 hours before gastroscopy.
In addition, in our study, there was no significant difference in the gastric emptying time or volume of residual gastric fluid in volunteers who drank 500 mL of water and 787.31±166.82 mL of water, which is a confusing result. We speculate that the emptying speed in gastric tissue varies according to the volume, leading to this result. The specific cause of this phenomenon needs to be confirmed by additional experiments.
In summary, if an individual does not have abnormal gastric movements and does not drink more than 1,000 mL of water, it is safe for them to stop drinking liquid 2 hours before a gastroscopy examination. Stopping drinking more than 2 hours before the test is not necessary and increases the risk of stress responses such as thirst, anxiety, and irritability.
Acknowledgments
Funding: This manuscript was supported by Bethune Foundation for Excellence (HZB-20181119-16).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/dmr-20-64
Data Sharing Statement: Available at http://dx.doi.org/10.21037/dmr-20-64
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr-20-64). All authors report grants from Bethune Aixikang Distinguished Surgical Fund project, during the conduct of the study. Dr. CZ serves as an unpaid associate editor-in-chief of Digestive Medicine Research.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of the Seventh Affiliated Hospital of Sun Yat-sen University (No.: KY-2021-024-01). Informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Trummel J. Sedation for gastrointestinal endoscopy: the changing landscape. Curr Opin Anaesthesiol 2007;20:359-64. [Crossref] [PubMed]
- Frieling T, Heise J, Kreysel C, et al. Sedation-associated complications in endoscopy--prospective multicentre survey of 191142 patients. Z Gastroenterol 2013;51:568-72. Erratum in: Z Gastroenterol 2013;51:E1. [Crossref] [PubMed]
- McCracken GC, Montgomery J. Postoperative nausea and vomiting after unrestricted clear fluids before day surgery: A retrospective analysis. Eur J Anaesthesiol 2018;35:337-42. [Crossref] [PubMed]
- Kyrtatos PG, Constandinou N, Loizides S, et al. Improved patient education facilitates adherence to preoperative fasting guidelines. J Perioper Pract 2014;24:228-31. [Crossref] [PubMed]
- Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev 2003;CD004423 [Crossref] [PubMed]
- . Major Adverse Events and Relationship to Nil per Os Status in Pediatric Sedation/Anesthesia outside the Operating Room: A Report of the Pediatric Sedation Research Consortium: Erratum: Erratum. Anesthesiology 2019;130:670. Erratum for Anesthesiology 2016;124:1202. [Crossref] [PubMed]
- Green SM, Mason KP, Krauss BS. Pulmonary aspiration during procedural sedation: a comprehensive systematic review. Br J Anaesth 2017;118:344-54. [Crossref] [PubMed]
- . Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology 2017;126:376-93. [Crossref] [PubMed]
- Thomas M, Morrison C, Newton R, et al. Consensus statement on clear fluids fasting for elective pediatric general anesthesia. Paediatr Anaesth 2018;28:411-4. [Crossref] [PubMed]
- Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 2011;28:556-69. [Crossref] [PubMed]
- Callaghan JL, Neale JR, Boger PC, et al. Variation in preparation for gastroscopy: lessons towards safer and better outcomes. Frontline Gastroenterol 2016;7:187-90. [Crossref] [PubMed]
- Horosz B, Nawrocka K, Malec-Milewska M. Anaesthetic perioperative management according to the ERAS protocol. Anaesthesiol Intensive Ther 2016;48:49-54. [Crossref] [PubMed]
Cite this article as: Li J, Liu Y, Lin H, Huang J, Zhang C. Feasibility study of shortening the no drinking time before gastroscopy to two hours. Dig Med Res 2021;4:1.


