Hepatic portal venous gas associated with bowel necrosis: report of one case and literature review
Introduction
Hepatic portal venous gas (HPVG) is a rare imaging finding. It can be associated with mesenteric ischemia in most cases, and these patients typically have a poor prognosis and at elevated risk of death. Meanwhile, the detection rate of HPVG is also rising in some patients with non-ischemic diseases. In recent years, more HPVG cases have been detected with the help of computed tomography (CT), which has improved the clinical prognosis of patients with mesenteric ischemia. In this article, we described a case of HPVG associated with intestinal necrosis and performed a literature review in terms of epidemiology, etiology, diagnostic criteria, and treatment.
Case presentation
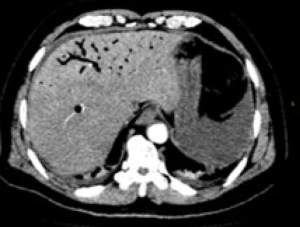
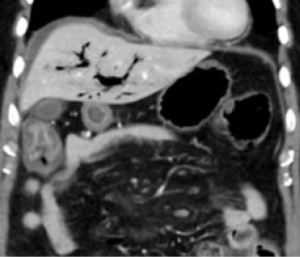
A 70-year-old male patient was admitted due to “abdominal distension and abdominal pain for 11 hours”. The symptoms occurred after the patient ate frozen watermelon 11 hours ago. The patient also experienced nausea (but without vomiting) and blood in the stool. He presented to the emergency department of our hospital for evaluation. He had an earlier history of cerebral infarction, for which he has been treated with daily aspirin. Physical examination showed a respiratory rate (R) of 20 times/min, a pulse rate (P) of 110 times/min, and blood pressure (BP) of 155/98 mmHg. He was mentally conscious, but with a characteristic face of acute illness. Abdominal bloating was obvious, along with abdominal tenderness, rebound pain, and muscle tension. Bowel sounds disappeared. Laboratory tests showed: white blood cell count (WBC), 15.54×109 cells/L; percentage of neutrophils (N), 91.6%; hemoglobin (Hb), 165 g/L; platelets (PLT), 154×109 cell/L; procalcitonin (PCT), >10 ng/mL. Contrast-enhanced CT of the chest and abdomen revealed that: (I) abundant gas accumulated in the intestinal canal; thickening and edema were visible on the walls of ileum and ascending colon; in particular, the wall of the right half of the colon was remarkably thickened, with reduced enhancement. It was speculated that the gas penetrated the intestinal walls and caused diffuse gas accumulation in the abdominal cavity after the infection and edema of the colon and small intestine and the perforation of the locally diseased intestines (including the transverse colon) and the posterior wall of the gastric antrum. (II) The gas accumulation in the portal vein of the liver and the diffuse gas accumulation in the branches of the mesenteric vein (mainly the superior mesenteric vein) were observed, which might be caused by an intestinal infection. Bacteremia might be possible (Figures 1,2). Emergency surgery was performed after admission. During the operation, a large volume of bloody turbid ascites was seen in the abdominal cavity. About 50 cm of the small intestine had no motility and developed ischemic and necrotic about 40 cm away from the ileocecal valve. Based on intraoperative findings including small intestinal necrosis, acute diffuse peritonitis, and massive ascites, resection of small necrotic intestine plus intestinal anastomosis was performed. Postoperative recovery was smooth, and the patient was discharged 20 days after surgery.
Discussion
HPVG is an ominous radiologic sign, proposed by Wolfe and Evens in 1955 (1). HPVG is associated with a variety of abdominal diseases, ranging from benign diseases to surgical emergencies requiring prompt intervention, including intestinal necrosis (72%), ulcerative colitis (8%), intraabdominal abscess (6%), small bowel obstruction (3%), and gastric ulcers (3%) (2). The pathogenesis of HPVG is still unknown. The possible causes of HPVG may include: (I) gas from the intestinal lumen can travel to the portal vein and then into the liver, and (II) gas-forming organisms gain entry into the portal venous system, and the gas enters the liver along with blood circulation (2). The diagnosis of HPVG is usually made by plain abdominal radiography, sonography, color Doppler flow imaging, or computed tomography (CT) scan. CT is regarded as the gold standard. On CT images, HPVG is characteristically associated with peripheral gas lucencies, which are noted even within the last 2 cm beneath the liver capsule. This peripheral gas distribution is related to the direction of blood flow into the liver. Also, a CT scan can show gas in the bowel wall (pneumatosis intestinalis) and the extrahepatic portal vein or its splanchnic vasculature (3). With the development of highly advanced imaging techniques such as CT and ultrasound, HPVG is diagnosed at much earlier stages and the prognosis has been improved. The mortality rates have decreased from 75–80% to 25–35% (4-7). Treatment of HPVG has long been controversial. The past decade has seen the dramatic change in the treatment concepts—from open surgery in the early years to the current conservative treatments featured by anti-infection and observation. The key factors affecting clinical decision-making include the presence of intestinal ischemia or necrosis and the patient’s condition (8). When HPVG is revealed on CT images, patients with clinically suspected intestinal ischemia or necrosis must undergo an emergency laparotomy. In patients without intestinal ischemia, proper treatment of the underlying disease typically can achieve a better prognosis and avoid unnecessary laparotomy. If imaging suggests the presence of HPVG, the patient should undergo detailed medical history-taking and physical examination, to learn the underlying conditions of the patient and thus pay the way for laparotomy.
Summary
HPVG is an ominous radiologic sign. Its early detection rate has continuously increased with the full application of CT and other imaging techniques. Notably, HPVG is not by itself a surgical indication, and the treatment depends on the underlying disease. The prognosis is related to the pathology itself and is not influenced by the presence of HPVG.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2020.01.02). The authors have no conflicts of interest to declare.
Ethical Statement: All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee(s) and with the Helsinki Declaration (as revised in 2013). We have obtained written consent from the patient to publish this case report and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wolfe JN, Evans WA. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am J Roentgenol Radium Ther Nucl Med 1955;74:486-8. [PubMed]
- Liebman PR, Patten MT, Manny J, et al. Hepatic--portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg 1978;187:281-7. [Crossref] [PubMed]
- Chirica M, Scatton O. Air in the portal venous system: radiologic differential diagnosis and etiology-specific treatment. J Chir (Paris) 2006;143:141-7. [Crossref] [PubMed]
- Cambria RP, Margolies MN. Hepatic portal venous gas in diverticulitis: survival in a steroid-treated patient. Arch Surg 1982;117:834-5. [Crossref] [PubMed]
- Benson MD. Adult survival with intrahepatic portal venous gas secondary to acute gastric dilatation, with a review of portal venous gas. Clin Radiol 1985;36:441-3. [Crossref] [PubMed]
- Faberman RS, Mayo-Smith WW. Outcome of 17 patients with portal venous gas detected by CT. AJR Am J Roentgenol 1997;169:1535-8. [Crossref] [PubMed]
- Iannitti DA, Gregg SC, Mayo-Smith WW, et al. Portal venous gas detected by computed tomography: is surgery imperative? Dig Surg 2003;20:306-15. [Crossref] [PubMed]
- Hou SK, Chern CH, How CK, et al. Hepatic portal venous gas: clinical significance of computed tomography findings. Am J Emerg Med 2004;22:214-8. [Crossref] [PubMed]
Cite this article as: Chen H, Zhan S, Deng Q, Hong C, Chen J, Yang S, Yu H, Wu W. Hepatic portal venous gas associated with bowel necrosis: report of one case and literature review. Dig Med Res 2020;3:5.