A rare cause of elbow stiffness after internal fixation of proximal ulna fracture: a case report of heterotopic ossification
Introduction
Olecranon fractures comprise approximately 10% of all fractures around the elbow (1). They vary in their complexity from relatively straightforward transverse fractures to comminuted and unstable configurations. As in other articular fractures, the aims of treatment, as defined by the AO group, are to restore the articular surface, achieve absolute stability of the fracture, and commence early active motion, and, finally, the restoration of function without pain (2,3).
This is only possible with ORIF (open reduction and internal fixation) such as TBW (tension band wiring), plate and intramedullary fixation techniques as well as fragment excision with triceps advancement (4-8). The TBW described by Weber and Vasey (3) has been widely used in the ORIF of olecranon, however, plate fixation has been used principally for the management of comminuted olecranon fractures in which TBW is not appropriate (4). Plates are generally applied to the dorsal surface of the ulna because this is the tension side of the olecranon which makes the construct most biomechanically sound, and because screws can be passed into the coronoid (9,10).
Anatomically contoured locking plates are one of the newest developments in olecranon plate technology and are being marketed as offering superior fixation as a result of the fixed angle construct (5).
Whilst good results have been shown with the use of these plates, there is currently insufficient evidence to suggest they are superior to other forms of plate fixation (5,11).
This report describes heterotopic ossification (HO) as a complication related to the internal fixation of a proximal ulna comminuted fracture.
Case presentation
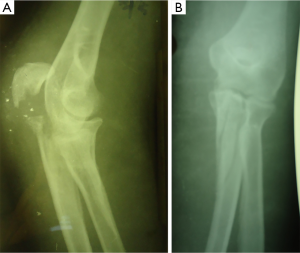
A 35-year-old, right-hand–dominant woman fell from a height sustaining an intra-articular, comminuted, fracture of the left proximal ulna (Figure 1). As shown in Figure 1, direct forces generated comminution (fragmentation) of the central portion of the proximal part of ulna including olecranon articular surface and, also avulsions of the coronoid process including the extension of the ulna shaft. The triceps brachii inserted into the posterior third of the olecranon and the proximal ulna separated the olecranon, the brachialis inserted into the coronoid process of the ulna produces tensile forces across the elbow joint during contraction, so as to separate the coronoid, thus resulting in complex fracture of proximal ulna and severe dysfunction of the elbow.
There was no abnormal findings in her medical, family and psycho-social history including relevant genetic information.
According to the AO principle of articular fracture management, ORIF using anatomical locking plate was performed, one day after the injury, without any complication.
Surgical technique
A direct reduction was performed using hooks, pointed reduction forceps, and K-wires. With exposure of the major fragments under direct vision, reduction was achieved and maintained with temporary pin fixation. The fracture reduction was visualized on each of the sigmoid notch and dorsally. Visualization of the coronoid could be made through the fracture site of the separated olecranon fragments before reduction.
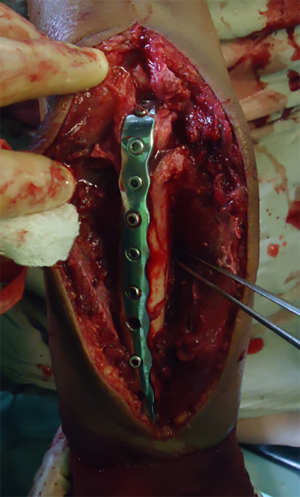
After reduction and temporary fixation, a posterior locking plate 3.5 which was contoured to the anatomical shape of proximal ulna was applied for this comminuted fractures.
Coronoid process was fixed with 3 screws and subsequent bicortical screws were placed in a locking plate (Figure 2).
Postoperative management
No external device like a dorsal splint was applied. The patient was started on an early rehabilitation program. The patient was allowed to use her elbow as tolerated. Active assisted exercises are started the day after, including gravity assisted elbow flexion with the patient lying supine.
At approximately 8 weeks the evidence of union was revealed on plain radiograph, but she didn`t recover her functional range of elbow motion, although professional physical therapy was applied.
She subsequently developed progressive elbow stiffness that was resistant to formal therapy.
At 16 weeks after surgery, his elbow flexion arc was not returned to functional range yet, ROM was 45° to 100°. Physical examination showed a loss of about 45° of extension, and about 50° of flexion compared with the uninjured side. Forearm rotation was maintained.
Radiographs taken at 6 months showed a union of proximal ulna and also profound heterotopic ossification posteriorly within the triceps muscle just over the olecranon and posterior to olecranon fossa within the triceps muscle (Figure 3).
Revision surgery & final results
Six months after the initial procedure we performed the second surgery, which included removal of plate and screws and excision of heterotopic ossification at the same time.
Intraoperatively we could find the 2 cm long bony mass surrounding the first and second screw hole of plate on the olecranon. Intraoperatively, we confirmed a full passive range of movement under anaesthesia (Figure 4).

Postoperative radiographs confirmed that the entire mass has been excised. 75 mg indomethacin was prescribed daily for 6 weeks after the second surgery. The patient started a regimen of active assisted elbow movements from the second postoperative day.
She was pain-free and obtained functional range of motion 3 weeks after the second procedure.
Two months after revision surgery, the patient was asymptomatic and had regained a range of elbow motion from 20° to 130°. The functional assessment revealed possibilities for global nutrition (hand-mouth), hygiene (hand-face) and grooming (hand-neck). On the basis of plain radiographic findings, we didn’t find any sign of recurrent ossification after an 18-month follow-up period. The evaluation of 24-month follow-up period showed relief of pain and maintenance of functional range of motion (Figure 5).

At the final follow-up, there was no adverse and unanticipated events.
- Injury on the 15th Dec. 2015.
- ORIF and then early rehabilitation program.
- Postop.8th week—union, but not enough elbow ROM.
- Postop.8th week—ROM 45° to 100°.
- Postop.6th month—union of proximal ulna and also profound heterotopic ossification posteriorly within the triceps muscle just over the olecranon.
- Second procedure which included removal of implants and excision of heterotopic ossification.
- Indomethacin administration.
- Postop.8th month (2 months after revision surgery)—elbow ROM 20° to 130°.
- Postop.18th month—not any sign of recurrent ossification.
- Postop.24th month—relief of pain and maintenance of functional ROM, no adverse and unanticipated events.
Discussion
The functional outcome following olecranon fracture fixation is generally good or excellent whatever method of fixation is used. The main complication following internal fixation of olecranon fractures is related to irritation caused by hardware.
Loss of motion is commonly encountered with patients typically losing 10°–15° of extension. The loss of elbow motion is worse in cases associated with fractures of the radial head, capitellum, coronoid or Monteggia fracture-dislocations (12,13).
The majority of patients recover a functional range of motion, frequently with small losses of extension, usually with no associated disability.
Previous studies of proximal ulna comminuted fracture, however, to our knowledge, have reported no cases of HO as a complication, despite the potential development of ectopic bone in the elbow.
Heterotopic ossification (HO), which is first described by Patin in 1962, is the formation of mature lamellar bone in nonosseous tissue. It is also termed heterotopic bone or ectopic osteogenesis (ossification and calcification). The most common cause of HO is trauma such as musculoskeletal injury, surgical trauma, or warfare injuries. When it forms outside the joint capsule and periosteum, it causes pain, swelling and is usually associated with limited range of motion. that is why, this is an important problem throughout orthopaedic surgery (14-24).
Heterotopic ossification may follow intracranial damage and is made more likely by delayed fixation and by passive stretching of the elbow (25).
It was reported that HO developed in approximately 3% of patients with a local injury of the elbow (26-29), and Elbow HO occurs in 20% of patients with Traumatic Brain Injury and forearm fractures (27,30-32).
Otherwise, Robert W. Wysocki (33) reported a case of triceps muscle ectopic ossification and resultant elbow stiffness after application of recombinant human bone morphogenetic protein to a distal humerus nonunion site. This case was directly related to the use of OP-1.
Most investigators agreed that the most frequent cause of heterotopic bone about the elbow is direct trauma, however, HO after ORIF of proximal ulna has not been reported yet, to our knowledge.
So now we are reporting a case of HO affecting the elbow motion after ORIF of proximal ulna comminuted fracture.
According to Hastings and Graham (27), this case seems class IIA.
In the present case we have experienced a complication of massive HO within the triceps directly over the olecranon where anatomical locking plate was lied, leading to marked loss of elbow motion. We believe that anatomical locking plate fixation is much superior over other techniques, but this unpredicted complication which was directly related to the operation developed.
The internal fixation in the present case has been rigid enough to ensure stability of fracture site, but we guess that the microtrauma caused by friction between the plate and triceps may have been the main factor. After operation we allowed the patient to use her elbow as tolerated, and then formal physical therapy which was thought to aggravate the injury caused by incision and muscular dissection.
This is supported by the pattern and extent of the ectopic bone that formed in this case.
Furthermore, we’ve not taken any measure to prevent the HO, which could be also a cause of this unique case, to our knowledge.
Careful handling of tissue during any surgical procedure, especially around the hip and elbow, is also of importance to minimize any trauma and subsequent inflammation. But the role of proper surgical technique in the formation of heterotopic bone is difficult to quantitate, so various preventive modalities of HO have been discussed in the literature (34).
Different modalities used include diphosphonates, etidronate, and NSAID’s such as indomethacin and naproxen. radiotherapy, Noggin, a BMP inhibitor, pulsed electromagnetic fields (PEMF), and free radical scavengers and N-acetylcysteine (35-39).
But we’ve not taken any the abovementioned measures because this complication has been very rarely reported. We thought postoperative therapy was not proper in this case, either. The principal of the HO treatment is appropriate immobilization for immature bone and physical therapy for a mature mass (38).
Just only focusing on the early motion of the injured elbow was more likely to promote the development of HO.
In the present case, we wonder if immobilization for 3–4 weeks rather than early motion would be beneficial. Although early motion and manipulation has been essential to prevent stiffness and has been reported to improve range of elbow motion, in this case they may have predisposed to hematoma formation, scarring, and heterotopic ossification.
From this experience, we do not recommend isolated physical therapy in patients with elbow injury, rather we recommend combined physical therapy with other preventive measures. Many authors agree that if ectopic bone around the elbow is causing or contributing to a loss of functional elbow motion, an operative procedure is warranted to remove the offending bone and release the joint capsule whether the motion limitation is partial or complete (ankylosis) (16,27).
Results of surgical excision of heterotopic ossification about the elbow have shown significant improvement in range of motion, independence, and quality of life in most cases (40-44).
They suggest that patients usually regain a full active range of motion within a few days of excision of the bony mass (21,24). In this case, the result of surgical excision was similar to the previous data.
The patient was pain-free and obtained functional range of motion 3 weeks after the second procedure.
Although this is a very rare case, we recommend that postoperative therapy should be performed with caution in the elbow where formation of excess bone restrict motion. Unless the recovery of functional ROM is achieved as predicted, HO should be doubted, refraining from passively stretching the injured elbow.
In order to prevent postoperative HO, intraoperatively, surgical dissection should be performed as carefully as possible, and postoperative, management should involve all effective measures such as abovementioned ones.
The patient felt satisfactory about her final outcome of the treatment and consent to this case report.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2020.01.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rommens PM, Kuchle R, Schneider RU, et al. Olecranon fractures in adults: factors influencing outcome. Injury 2004;35:1149-57. [Crossref] [PubMed]
- Mueller ME, Allgower M, Schneider R. Manual of internal fixation: techniques recommended by the AO-ASIF group, 3rd ed., Berlin, Germany: Springer–Verlag; 1991:1-158.
- Weber BG, Vasey H. Osteosynthese bei Olecranonfraktur. Unfallmedizinische Berufskrankheiten 1963;2:90-6.
- Anderson ML, Larson AL, Merton SM, et al. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma 2007;21:386-93. [Crossref] [PubMed]
- Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res 1992;229-35. [PubMed]
- Lavigne G, Baratz M. Fractures of the olecranon. J Am Soc Surg Hand 2004;4:94-102. [Crossref]
- Nowinski RJ, Nork SE, Segina DN, et al. Comminuted fracture-dislocations of the elbow treated with an AO wrist fusion plate. Clin Orthop 2000;238-44. [Crossref] [PubMed]
- Wolfgang G, Burke F, Bush D, et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res 1987;192-204. [PubMed]
- Bailey CS, MacDermid J, Patterson SD, et al. Outcome of plate fixation of olecranon fractures. J Orthop Trauma 2001;15:542-8. [Crossref] [PubMed]
- Simpson NS, Goodman LA, Jupiter JB. Contoured LC–DC plating of the proximal ulna. Injury 1996;27:411-7. [Crossref] [PubMed]
- Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg 2000;8:266-75. [Crossref] [PubMed]
- Ring D, Jupiter JB. Fracture dislocation of the elbow. J Bone Joint Surg Am 1998;80:566-80. [Crossref] [PubMed]
- Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury 2009;40:575-81. [Crossref] [PubMed]
- Jupiter JB, O’Driscoll SW, Cohen MS. The assessment and management of the stiff elbow. Instr Course Lect 2003;52:93-111. [PubMed]
- Furukawa K. Pharmacological aspect of ectopic ossification in spinal ligament tissues. Pharmacol Ther 2008;118:352-8. [Crossref] [PubMed]
- Tonbul M, Ozen S, Tonbul AT. Bilateral simultaneous heterotopic ossification of the reflected head of rectus femoris muscle: a case report and review of the literature. Case Rep Orthop 2014;2014:497075. [Crossref] [PubMed]
- Zimmermann SM, Würgler-Hauri CC, Wanner GA, et al. Echinomycin in the prevention of heterotopic ossification - an experimental antibiotic agent shows promising results in a murine model. Injury 2013;44:570-5. [Crossref] [PubMed]
- Chouhan DK, Dhillon M, Bachhal V, et al. Atraumatic heterotopic ossification of iliopsoas muscle: a case report. Orthop Surg 2012;4:197-201. [Crossref] [PubMed]
- Onder K, Muhammed B, Saime U, et al. Post-traumatic heterotopic ossification of the crus. A case study. Ortop Traumatol Rehabil 2011;13:299-301. [PubMed]
- Hsu JE, Keenan MA. Current review of heterotopic ossification. J Orthop 2010;20:126-30.
- McCulloch PC, Bush-Joseph CA. Massive heterotopic ossification complicating iliopsoas tendon lengthening: a case report. Am J Sports Med 2006;34:2022-5. [Crossref] [PubMed]
- Ahrengart L. Periarticular heterotopic ossification after total hip arthroplasty. Risk factors and consequences. Clin Orthop Relat Res 1991;49-58. [PubMed]
- Ritter MA, Vaughan RB. Ectopic ossification after total hip arthroplasty. Predisposing factors, frequency, and effect on results. J Bone Joint Surg 1977;59:345-51. [Crossref] [PubMed]
- Thorseth K. A case of traumatic myositis ossificans in the iliopsoas muscle. Acta Orthop Scand 1968;39:73-5. [Crossref] [PubMed]
- Summerfield SL, DiGiovanni C, Weiss AP. Heterotopic ossification of the elbow. J Shoulder Elbow Surg 1997;6:321-31. [Crossref] [PubMed]
- Garland DE, Blum C, Waters R. Periarticular Heterotopic Ossification in Head Injured Adults. J Bone Joint Surg 1980;62:1143-6. [Crossref] [PubMed]
- Hastings H, Graham T. The Classification and Treatment of Heterotopic Ossification about the Elbow and Forearm. Hand Clin 1994;10:417-37. [PubMed]
- Peterson SL, Mani MM, Crawford CM, et al. Postburn Heterotopic Ossification: Insights for Management Decision Making. J Trauma 1989;29:365-9. [Crossref] [PubMed]
- Thompson HC, Garcia A. Myositis Ossificans: Aftermath of Elbow Injuries. Clin Orthop 1967;129-34. [PubMed]
- Cohen MS. Heterotopic ossification of the elbow. In: Jupiter JB, ed. The stiff elbow. Rosemont: American Academy of Orthopaedic Surgeons, 2006:31-40.
- Garland DE, O'Hollaren R. Fractures and Dislocations about the Elbow in the Head-injured Adult. Clin Orthop 1982;38-41. [PubMed]
- Garland DE, Dowling V. Forearm Fractures in the Head-Injured Adult. Clin Orthop 1983;190-6. [PubMed]
- Wysocki RW, Cohen MS. Ectopic ossification of the triceps muscle after application of bone morphogenetic protein-7 to the distal humerus for recalcitrant nonunion: a case report. J Hand Surg Am 2007;32:647-50. [Crossref] [PubMed]
- Baird EO, Kang QK. Prophylaxis of heterotopic ossification - an updated review. J Orthop Surg Res 2009;4:12. [Crossref] [PubMed]
- Bek D, Beksaç B, Della Valle AG, et al. Aspirin decreases the prevalence and severity of heterotopic ossification after 1-stage bilateral total hip arthroplasty for osteoarthrosis. J Arthroplasty 2009;24:226-32. [Crossref] [PubMed]
- Vavken P, Castellani L, Sculco TP. Prophylaxis of heterotopic ossification of the hip: systematic review and meta-analysis. Clin Orthop Relat Res 2009;467:3283-9. [Crossref] [PubMed]
- Pakos EE, Tsekeris PG, Paschos NK, et al. The role of radiation dose in a combined therapeutic protocol for the prevention of heterotopic ossification after total hip replacement. J BUON 2010;15:74-8. [PubMed]
- Banovac K. The effect of etidronate on late development of heterotopic ossification after spinal cord injury. J Spinal Cord Med 2000;23:40-4. [Crossref] [PubMed]
- McAuliffe J. Early Excision of Heterotopic Ossification about the Elbow followed by Radiation Therapy. J Bone Joint Surg 1997;79:749-55. [Crossref] [PubMed]
- Djurickovic S, Meek RN, Snelling CF, et al. Range of Motion and Complications after Postburn Heterotopic Bone Excision about the Elbow. J Trauma 1996;41:825-30. [Crossref] [PubMed]
- Garland DE. A Clinical Perspective on Common Forms of Acquired Heterotopic Ossification. Clin Orthop 1991;13-29. [PubMed]
- Garland DE. Surgical Approaches for Resection of Heterotopic Ossification in Traumatic Brain-injured Adults. Clin Orthop 1991;59-70. [PubMed]
- Garland DE, Hanscom DA, Keenan MA, et al. Resection of Heterotopic Ossification in the Adult with Head Trauma. J Bone Joint Surg Am 1985;67:1261-9. [Crossref] [PubMed]
- Kolessar DJ, Katz SD, Keenan ME. Functional Outcome Following Surgical Resection of Heterotopic Ossification in Patients with Brain Injury. J Head Trauma Rehabil 1996;44:4.
Cite this article as: Mun CS, So TS, Jang CH. A rare cause of elbow stiffness after internal fixation of proximal ulna fracture: a case report of heterotopic ossification. Dig Med Res 2020;3:9.