Combined laparoscopic colectomy and splenectomy for bleeding transverse colon cancer and MDS associated splenomegaly with refractory ITP
Introduction
We recently reported a combined laparoscopic splenectomy and colectomy for unrelated pathologies including sigmoid diverticulitis and granulomatous splenic lesions due to sarcoidosis (1). Combined splenectomy with resection of left colon, sigmoid colon or rectum is usually due to injury of the spleen causing un-controllable hemorrhage during mobilization of the splenic flexure (2). Much less common indications include multivisceral resection in case of locally advanced malignancies of pancreatic tail or splenic colon flexure or in case of trauma to the area (3,4). Only few cases of such combined procedures for independent pathologies have been published.
Case presentation
A 72-year-old male with multiple medical issues was referred for possible surgical treatment including splenectomy for immune thrombocytopenic purpura (ITP) and/or transverse colectomy for bleeding colon cancer. The patient had been diagnosed with ITP in 2003. The disorder was initially poorly responsive to steroids and IVIG. Platelet count remained stable between 30 and 50 K for a decade and therefore, no specific therapy was given. However, in 2014 his platelet count dropped below 30,000. Repeat Bone marrow biopsy in January 2015 showed increased number of megakaryocytes some with dysplasia with trisomy 8 on 30% of metaphases by cytogenetics establishing diagnosis of myelodysplastic syndrome (MDS).
Rituximab (Rituxan) monotherapy was given followed by high dose dexamethasone in combination with low dose Cyclosporine A and weekly Rituximab with temporary response. Eltrombopag (Promacta) also only had transient response. Danazol was started achieving a significant response in his platelet count, however had to be discontinued as he developed recurrent deep soft tissue and muscle bleedings with impending compartment syndrome. The thrombocytopenia worsened and he had repeat bone marrow biopsy and SNP showing progression of the MDS with acquisition of new mutations. He also developed mild anemia but decision was made not to treat his MDS with hypomethylating agents due to fear of more side effects and worsening cytopenia.
Subsequently, in 2018 he developed significantly worsening anemia with iron deficiency. Workup showed a distal transverse colon mass with liver lesions. Liver biopsy showed metastatic colon adenocarcinoma that was MSI high, BRAF v600e mutated, KRAS wild with normal Her2. He was treated with low dose FOLFOX without avastin achieving a major response in the liver and at the primary site at the expense of severe cytopenia requiring RBC and Platelet transfusions. The course was complicated by severe protracted hematochezia and Romiplostim (N Plate) and later Fostamatinib (Tavalisse) were tried without response.
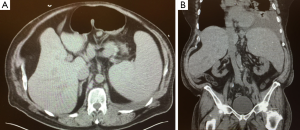
As palliative radiation to the primary colon tumor bleeding site did not stop the hemorrhage and as his clinical condition rapidly deteriorated, surgical evaluation for palliative colectomy and possible removal of the large spleen (Figure 1) was obtained. At the time platelet count was 4K, the patient had left lower lobe pneumonia with a large pleural effusion (Figure 1B) and interventional radiology refused to place a pig-tail due to the bleeding risk; in addition he was obese and diabetic using an insulin pump. After lengthy discussion with the patient and the other involved teams, surgery with resection of the colon segment harboring the bleeding source together with splenectomy was offered and a minimal invasive approach would be attempted.
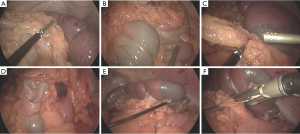
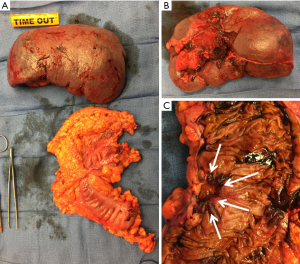
Access to the abdomen was achieved using the Fios 1st entry port in the left upper quadrant and pneumoperitoneum was established. Additional ports were placed and the abdomen was explored revealing the very large spleen (Figure 2A) but no carcinomatosis and no visible liver metastases. Platelet count at start of surgery was 4 K/mL. The spleen (25 cm in length) was mobilized by dividing the gastrocolic ligament and short gastric vessels followed by the splenocolic ligament and the lateral attachments as far up as possible using the EnSeal (Figure 2A). The tumor at the distal transverse colon was visualized (Figure 2B) and the omentum 10 cm proximal to the tumor was split (Figure 2C). The splenic flexure and descending colon were completely mobilized, a window was created in the mesocolon (Figure 2D) followed by division of the mesentery at the base. The splenic hilum at the lower pole was divided using the Enseal and two loads of the Echelon stapler (Figure 2E,F). At this point the 1st platelet concentrate was infused. The main hilum was too bulky for safe laparoscopic division as the stapler would not open far enough to capture the tissue. During further manipulation using a sponge to pull the spleen up a bleed occurred, which was tamponaded. Additional laparoscopic dissection was attempted but found to be technically impossible due to the size of the organ. A 10 cm epigastric incision was made and a wound protector placed. The hilar vessels were divided using a hand assisted technique inserting the stapler through a 10–12 mm port or the mini-incision. The spleen was removed through the mini-incision and two additional platelet concentrates were transfused. The splenic flexure was brought out and the colon was resected and anastomosed using a two staple load technique with a 75 mm GIA. Total operative time was 155 minutes. Pathology (Figures 3) demonstrated splenomegaly with signs of ITP and a T3N2M1 colon adenocarcinoma (known liver metastases). Platelet count in the wake up area after 2 hours exceeded 200 K and the patient was returned extubated and stable to the floor. The next day, the 3,000 mL opaque pleural effusion was drained with a Pigtail. Antibiotics for his pneumonia were continued and standard post splenectomy immunization was administered. Bowel function returned within 48 hours; the patient was discharged after 5 days and had no major complications. He was well at the 4 weeks follow up, however, withdrew care and died within few days.
Discussion
Only few patients have an indication for elective splenectomy together with segmental colectomy (1,3-5). A case like the one described herein has thus far not been published. In the case of profound ITP associated thrombocytopenia, naturally the risk for a bleed is significantly elevated. However, platelets cannot be given in ITP prior to division of the hilum as platelets are immediately pooled and lysed as long as there is blood supply to the organ. Partial splenectomy by embolization of the splenic artery may be an alternative to treat ITP (6). Splenectomy in MDS associated ITP is controversial as extramedullary hematopoiesis may be crucial in long term survival (7), however, in our case the refractory thrombocytopenia with ongoing bleed not amendable to another treatment left us with only this option. Removing only the cancer bearing colon would not have addressed the thrombocytopenia, which prohibited other interventions including drainage of the large pleural effusion. Taking only the spleen out on the other hand would have left the bleeding source, which could potentially have worsened with administration of avastin. In order to minimize bleeding and have best laparoscopic exposure for the most critical step of the procedure, the colon was completely mobilized prior to stapling of the hilum. The wide bulky hilum hindered completion of this step but a hand assisted technique without a large laparotomy was possible and done as soon as a bleed occurred. The opening of approximately 10 cm was used to extract the specimen as well as for the colon resection and extracorporeal anastomosis. Platelets immediately increased to 200 K but then came down during the next 2 weeks to <40 K before they stabilized around 100 K. Also the leucocytopenia resolved and WBC after 4 weeks was >10 K, however, his anemia lingered despite no more active bleeding.
The combined procedure can be safely performed using a laparoscopic approach (1).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2019.11.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kubicki N, Kavic S, Bonatti HJ. Laparoscopic sigmoid colectomy and splenectomy for diverticulitis and splenic sarcoidosis. J Minim Access Surg 2019;15:342-4. [Crossref] [PubMed]
- Masoomi H, Carmichael JC, Mills S, et al. Predictive factors of splenic injury in colorectal surgery: data from the Nationwide Inpatient Sample, 2006-2008. Arch Surg 2012;147:324-9. [Crossref] [PubMed]
- Kapur V, Krikhely M, Leitman IM. Operative management of splenic rupture and hepatic flexure injury during diagnostic colonoscopy in a patient with adenocarcinoma of the cecum. J Surg Case Rep 2015;2015:e9. [Crossref] [PubMed]
- Chen TC, Liang JT. Laparoscopic En Bloc Resection of T4 Colon Cancer Invading the Spleen and Pancreatic Tail. Dis Colon Rectum 2016;59:581-2. [Crossref] [PubMed]
- Kawamoto K, Teramoto T, Watanabe M, et al. Splenic abscess associated with colon cancer: a case report. Jpn J Clin Oncol 1993;23:384-8. [PubMed]
- Togasaki E, Shimizu N, Nagao Y, et al. Long-term efficacy of partial splenic embolization for the treatment of steroid-resistant chronic immune thrombocytopenia. Ann Hematol 2018;97:655-62. [Crossref] [PubMed]
- Bourgeois E, Caulier MT, Rose C, et al. Role of splenectomy in the treatment of myelodysplastic syndromes with peripheral thrombocytopenia: a report on six cases. Leukemia 2001;15:950-3. [Crossref] [PubMed]
Cite this article as: Bonatti H, Tang Y, Hamden H. Combined laparoscopic colectomy and splenectomy for bleeding transverse colon cancer and MDS associated splenomegaly with refractory ITP. Dig Med Res 2020;3:2.