
Laparoscopic total gastrectomy for gastric cancer with adult intestinal malrotation: a case report
Introduction
Intestinal malrotation is a rare congenital anomaly that results from failure of the normal rotation and fixation of the midgut around the axis of the superior mesenteric artery (SMA) during embryologic development. Approximately 90% are diagnosed with the onset of symptoms during the first year of life (1,2), but asymptomatic diagnosis in adults is uncommon.
When abdominal surgery is required in adult patients with asymptomatic intestinal malrotation, surgeons should carefully consider its anatomical differences (3). Especially when creating a Roux-en-Y reconstruction, a proper design of the Roux limb is crucial in avoiding twisting or obstruction of the intestine after surgery. We herein report a case of gastric cancer with an adult asymptomatic intestinal malrotation treated by laparoscopic total gastrectomy (LTG) while considering adequate design of Roux-en-Y reconstruction.
Case presentation
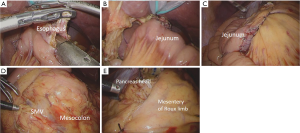
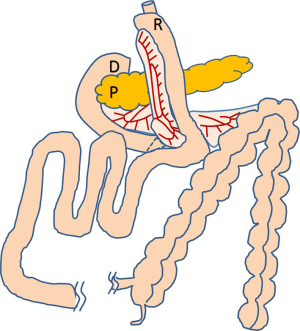
A 67-year-old man was referred to our hospital for further evaluation of gastric cancer detected after epigastric discomfort. Upper endoscopic examination showed a type 3 tumor on the posterior wall of the gastric corpus. Abdominal computed tomography (CT) showed several lymph node metastases, and a small amount of ascites with small peritoneal nodules. He was diagnosed with clinical stage IV gastric carcinoma, and platinum-fluoropyrimidine chemotherapy was started. After four cycles of chemotherapy, CT examination showed remarkable shrinkage of the main tumor and metastatic nodes as well as disappearance of the ascites and peritoneal nodules. Staging laparoscopy was performed and confirmed P0CY0 status; therefore, radical gastrectomy as conversion therapy was planned. During the staging laparoscopy, non-rotation type intestinal malrotation was detected incidentally. We retrospectively checked CT images and verified that the superior mesenteric vein (SMV) was located on the left side of the superior mesenteric artery (SMA), known as the “SMV rotation sign” and the whole colon was located on the left side and the jejunum on the right side of the patient (Figure 1A,B). Careful informed consent about laparoscopic surgery for advanced gastric cancer was obtained from the patient (4). LTG with spleen-preserving splenic hilar dissection was carried out. The usual C-shaped Roux limb appeared unnatural, presenting some risk of bowel twisting or obstruction. Finally, we designed a reverse C-shaped Roux limb that was more anatomically suitable. Intracorporeal esophagojejunostomy was done with a side-to-side overlap method as previously described (5,6), whereby the jejunum is anastomosed at the posterior wall of the esophagus. Usually in our procedure, a linear stapler is inserted from the right lower port; however, in this case it was introduced from the left lower port to adjust its axis to the jejunum. The common entry hole was closed by an interrupted hand-sewn suture as usual (Figure 2A,B). A jejunojejunostomy was made 40 cm distal from the esophagojejunostomy in side-to-side anti-peristaltic fashion, completing a reverse C-shaped Roux-en-Y reconstruction (Figure 2C). A mesenteric gap resulting from the jejunojejunostomy was closed as normal. Unusually, Petersen’s defect was not recognized because the mesentery of the transverse colon was dislocated to the right side of the patient. There was a small space between the anterior surface of the pancreas and the lifted Roux limb, but the closure appeared difficult, raising concern for pancreatic injury (Figure 2D,E). The completion schema of the reconstruction is shown in Figure 3. The operation time was 247 minutes and estimated blood loss 3 g. The postoperative course was uneventful, and the patient was discharged on the 8th postoperative day.

Discussion
As the incidence of intestinal malrotation diagnosed in adults has been reported as 0.2% to 1.0%, every clinical surgeon is open to the probability of encountering patients with this disease. Four subtypes of this disease are well known, namely, non-rotation type (only 90° rotation), malrotation type (only 180° rotation), reversed rotation type, and paraduodenal hernia (7), according to the status of rotational insufficiency. Non-rotation type, which was recognized in the current case, is reported as the most common subtype, accounting for around 50%. Nowadays, most cases of asymptomatic intestinal malrotation are diagnosed either incidentally during surgery or via an abdominal CT scan with specific findings (8). As the number of laparoscopic surgeries continues to increase, the importance of exploration of the abdominal cavity should be emphasized.
Usually the Roux limb is placed in a C-shaped position because the Treitz ligament is located on the left side of patients. In the current case, we placed the Roux limb in a reverse C-shape to achieve the natural contours. Lee et al. also reported using this reverse C-shaped Roux limb in a similar patient (9). For esophagojejunostomy they used a circular stapler, which was introduced from a mini-laparotomy on the right side of the patient. In the current case, we used a linear stapler in overlap mode, which is a standardized procedure in our institution. The completion view of the Roux-en-Y limb was very natural.
In patients with intestinal malrotation, prevention of postoperative bowel obstruction, torsion, or internal hernia is essential. In Roux-en-Y reconstruction under laparoscopic surgery, closure of the mesenteric gap or Petersen’s defect usually is thought to be mandatory in avoiding internal hernia. In the current case, Petersen’s defect was absent owing to dislocation of the transverse colon mesentery, which deviated to the left side. In this case it was impossible to suture the space between the jejunal limb and the retroperitoneum, although these decisions should be made according to the individual anatomical situation.
Published reports of laparoscopic gastric cancer surgery for adult intestinal malrotation are rare. To the best of our knowledge, our report is the second in the English language regarding LTG in a patient with intestinal malrotation. A previous report by Lee et al. also emphasized the efficiency of similar Roux-limb creation with an excellent postoperative course (9). Although such disease situations may be very rare, this method can be recommended for similar cases.
In conclusion, when performing LTG following Roux-en-Y reconstruction in patients with intestinal malrotation, an adequate Roux-limb design according to each situation is considered essential. A reverse C-shaped Roux limb is our recommended option.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/dmr.2018.06.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for whom identifying information is included in this article. This article does not contain any studies with human or animal subjects performed by any of the authors.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kapfer SA, Rappold JF. Intestinal malrotation-not just the pediatric surgeon's problem. J Am Coll Surg 2004;199:628-35. [Crossref] [PubMed]
- Husberg B, Salehi K, Peters T, et al. Congenital intestinal malrotation in adolescent and adult patients: a 12-year clinical and radiological survey. Springerplus 2016;5:245. [Crossref] [PubMed]
- Mateo R, Stapfer M, Singh G, et al. Pancreaticoduodenectomy in adults with congenital intestinal rotation disorders. Pancreas 2005;31:413-5. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4, in Japanese), Tokyo: Kanehara & Co., Ltd., 2014.
- Kinoshita T, Shibasaki H, Enomoto N, et al. Laparoscopic splenic hilar lymph node dissection for proximal gastric cancer using integrated three-dimensional anatomic simulation software. Surg Endosc 2016;30:2613-9. [Crossref] [PubMed]
- Inaba K, Satoh S, Ishida Y, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 2010;211:e25-9. [Crossref] [PubMed]
- Wang CA, Welch CE. Anomalies of intestinal rotation in adolescents and adults. Surgery 1963;54:839-55. [PubMed]
- Matzke GM, Dozois EJ, Larson DW, et al. Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc 2005;19:1416-9. [Crossref] [PubMed]
- Lee J, Lim JS, Cho I, et al. Laparoscopic total gastrectomy in a gastric cancer patient with intestinal malrotation. J Gastric Cancer 2013;13:188-91. [Crossref] [PubMed]
Cite this article as: Tonouchi A, Kinoshita T, Watanabe M, Sugita S, Kaito A, Tokunaga M. Laparoscopic total gastrectomy for gastric cancer with adult intestinal malrotation: a case report. Dig Med Res 2018;1:6.


